The Journal of Thoracic and Cardiovascular Surgery ( IF 6 ) Pub Date : 2022-06-01 , DOI: 10.1016/j.jtcvs.2022.05.032 Rolfy A Perez Holguin 1 , Elizabeth J Olecki 1 , William G Wong 1 , Kelly A Stahl 1 , Pauline H Go 2 , Matthew D Taylor 2 , Michael F Reed 2 , Chan Shen 3
|
Objective
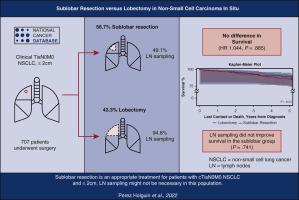
Guidelines for treatment of non–small cell lung cancer identify patients with tumors ≤2 cm and pure carcinoma in situ histology as candidates for sublobar resection. Although the merits of lobectomy, sublobar resection, and lymphoid (LN) sampling, have been investigated in early-stage non–small cell lung cancer, evaluation of these modalities in patients with IS disease can provide meaningful clinical information. This study aims to compare these operations and their relationship with regional LN sampling in this population.
Methods
The National Cancer Database was used to identify patients diagnosed with non–small cell lung cancer clinical Tis N0 M0 with a tumor size ≤2 cm from 2004 to 2017. The χ2 tests were used to examine subgroup differences by type of surgery. Kaplan-Meier method and Cox proportional hazard model were used to compare overall survival.
Results
Of 707 patients, 56.7% (401 out of 707) underwent sublobar resection and 43.3% (306 out of 707) underwent lobectomy. There was no difference in 5-year overall survival in the sublobar resection group (85.1%) compared with the lobectomy group (88.9%; P = .341). Multivariable survival analyses showed no difference in overall survival (hazard ratio, 1.044; P = .885) in the treatment groups. LN sampling was performed in 50.9% of patients treated with sublobar resection. In this group, LN sampling was not associated with improved survival (84.9% vs 85.0%; P = .741).
Conclusions
We observed no difference in overall survival between sublobar resection and lobectomy in patients with cTis N0 M0 non–small cell lung cancer with tumors ≤2 cm. Sublobar resection may be an appropriate surgical option for this population. LN sampling was not associated with improved survival in patients treated with sublobar resection.
中文翻译:

非小细胞原位癌亚肺叶切除术与肺叶切除术的结果
客观的
非小细胞肺癌治疗指南将肿瘤≤2cm且组织学纯原位癌的患者确定为亚肺叶切除术的候选者。尽管肺叶切除术、亚肺叶切除术和淋巴样 (LN) 取样的优点已在早期非小细胞肺癌中进行了研究,但对 IS 疾病患者的这些治疗方式进行评估可以提供有意义的临床信息。本研究旨在比较这些操作及其与该人群区域 LN 抽样的关系。
方法
美国国家癌症数据库用于识别2004年至2017年诊断为非小细胞肺癌临床Tis N0 M0且肿瘤大小≤2 cm的患者。χ 2 检验用于检查按手术类型划分的亚组差异。采用Kaplan-Meier法和Cox比例风险模型比较总生存期。
结果
在 707 名患者中,56.7%(707 名患者中的 401 名)接受了亚肺叶切除术,43.3%(707 名患者中的 306 名)接受了肺叶切除术。亚肺叶切除组 (85.1%) 与肺叶切除组 (88.9%; P = .341)相比,5 年总生存率没有差异。 多变量生存分析显示治疗组的总生存率没有差异(风险比,1.044;P = .885)。50.9% 接受亚肺叶切除治疗的患者进行了 LN 取样。在该组中,LN 取样与生存率改善无关(84.9% vs 85.0%;P = .741)。
结论
我们观察到,对于肿瘤≤2cm的cTis N0 M0非小细胞肺癌患者,亚肺叶切除术和肺叶切除术的总生存率没有差异。亚肺叶切除术可能是该人群的合适手术选择。淋巴结取样与接受亚肺叶切除术治疗的患者生存率的改善无关。



























 京公网安备 11010802027423号
京公网安备 11010802027423号