JACC: Heart Failure ( IF 13.0 ) Pub Date : 2022-05-30 , DOI: 10.1016/j.jchf.2022.04.003 Aniket S Rali 1 , Sagar Ranka 2 , Amy Butcher 3 , Zubair Shah 2 , Joseph E Tonna 4 , Marc M Anders 5 , Marshal D Brinkley 1 , Hasan Siddiqi 1 , Lynn Punnoose 1 , Mark Wigger 1 , Suzanne B Sacks 1 , Dawn Pedrotty 1 , Henry Ooi 1 , Matthew D Bacchetta 6 , Jordan Hoffman 7 , William McMaster 7 , Keki Balsara 7 , Ashish S Shah 7 , Jonathan N Menachem 1 , Kelly H Schlendorf 1 , JoAnn Lindenfeld 1 , Sandip K Zalawadiya 1
|
Background
As utilization of veno-arterial extracorporeal life support (VA-ECLS) in treatment of cardiogenic shock (CS) continues to expand, clinical variables that guide clinicians in early recognition of myocardial recovery and therefore, improved survival, after VA-ECLS are critical. There remains a paucity of literature on early postinitiation blood pressure measurements that predict improved outcomes.
Objectives
The objective of this study is to help identify early blood pressure variables associated with improved outcomes in VA-ECLS.
Methods
The authors queried the ELSO (Extracorporeal Life Support Organization) registry for cardiogenic shock patients treated with VA-ECLS or venovenous arterial ECLS between 2009 and 2020. Their inclusion criteria included treatment with VA-ECLS or venovenous arterial ECLS; absence of pre-existing durable right, left, or biventricular assist devices; no pre-ECLS cardiac arrest; and no surgical or percutaneously placed left ventricular venting devices during their ECLS runs. Their primary outcome of interest was the survival to discharge during index hospitalization.
Results
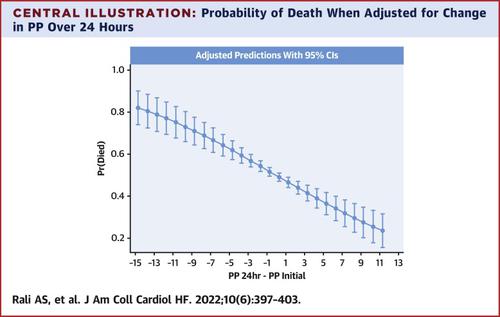
A total of 2,400 CS patients met the authors’ inclusion criteria and had complete documentation of blood pressures. Actual mortality during index hospitalization in their cohort was 49.5% and survivors were younger and more likely to be Caucasian, intubated for >30 hours pre-ECLS initiation, and had a favorable baseline SAVE (Survival After Veno-arterial ECMO) score (P < 0.05 for all). Multivariable regression analyses adjusting for SAVE score, age, ECLS flow at 4 hours, and race showed that every 10-mm Hg increase in baseline systolic blood pressure (HR: 0.92 [95% CI: 0.89-0.95]; P < 0.001), and baseline pulse pressure (HR: 0.88 [95% CI: 0.84-0.91]; P < 0.001) at 24 hours was associated with a statistically significant reduction in mortality.
Conclusions
Early (within 24 hours) improvements in pulse pressure and systolic blood pressure from baseline are associated with improved survival to discharge among CS patients treated with VA-ECLS.
中文翻译:

与 VA-ECLS 预后改善相关的早期血压变量
背景
随着静脉-动脉体外生命支持 (VA-ECLS) 在心源性休克 (CS) 治疗中的应用不断扩大,指导临床医生早期识别心肌恢复并因此提高 VA-ECLS 后生存率的临床变量至关重要。关于预测改善结果的早期开始后血压测量的文献仍然很少。
目标
本研究的目的是帮助确定与 VA-ECLS 预后改善相关的早期血压变量。
方法
作者在 ELSO(体外生命支持组织)登记处查询了 2009 年至 2020 年间接受 VA-ECLS 或静脉动脉 ECLS 治疗的心源性休克患者。他们的纳入标准包括接受 VA-ECLS 或静脉动脉 ECLS 治疗;没有预先存在的耐用右、左或双心室辅助装置;无 ECLS 前心脏骤停;在他们的 ECLS 运行期间没有手术或经皮放置左心室通气装置。他们感兴趣的主要结果是指数住院期间出院的存活率。
结果
共有 2,400 名 CS 患者符合作者的纳入标准,并有完整的血压记录。他们队列中指数住院期间的实际死亡率为 49.5%,幸存者更年轻,更可能是白种人,在 ECLS 开始前插管时间 > 30 小时,并且基线 SAVE(静脉-动脉 ECMO 后生存)评分良好( P <所有 0.05)。调整 SAVE 评分、年龄、4 小时 ECLS 流量和种族的多变量回归分析表明,基线收缩压每升高 10 mm Hg(HR:0.92 [95% CI:0.89-0.95];P < 0.001 ), 24 小时时的基线脉压和基线脉压(HR:0.88 [95% CI:0.84-0.91];P < 0.001)与死亡率在统计学上显着降低相关。
结论
在接受 VA-ECLS 治疗的 CS 患者中,脉压和收缩压较基线的早期(24 小时内)改善与出院存活率提高相关。


























 京公网安备 11010802027423号
京公网安备 11010802027423号