Acta Neuropathologica ( IF 12.7 ) Pub Date : 2022-05-12 , DOI: 10.1007/s00401-022-02432-5 Shih-Hsiu J Wang 1, 2 , Yuanyuan Guo 3 , John F Ervin 2 , Jay B Lusk 1, 2 , Sheng Luo 3
|
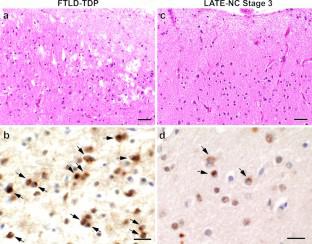
Limbic-predominant age-related TDP-43 encephalopathy neuropathological change (LATE-NC) is most often seen in the oldest-old (≥ 90 years of age) but can also be present in the younger-old (< 90 years of age). In this study, we compared the neuropathological associations of LATE-NC and contribution of LATE-NC to cognitive impairment between the oldest-old and younger-old. We observed significant differences in the prevalence of LATE-NC and its association with other co-pathologies in these two age groups. LATE-NC was present in 30.9% (34/110) of the oldest-old but only 9.4% (19/203) of the younger-old. Participants of the oldest-old with LATE-NC were more likely to have hippocampal sclerosis (HS) (55.9% vs. 10.5%, p < 0.001) and moderate to severe arteriolosclerosis (82.4% vs. 50%, p = 0.007), but not intermediate to high Alzheimer’s disease neuropathologic change (ADNC) (70.6% vs. 59.2%, p = 0.486) or Lewy body disease (LBD) (20.6% vs. 26.3%, p = 0.793). Participants of the younger-old with LATE-NC were more likely to have intermediate to high ADNC (94.7% vs. 55.4%, p < 0.001) and LBD (63.2% vs. 28.8%, p = 0.013) in addition to hippocampal sclerosis (42.1% vs. 6.5%, p < 0.001), and moderate to severe arteriolosclerosis (42.1% vs. 15.2%, p = 0.020). Of note, participants with LATE-NC and no to low ADNC were very rare in the younger-old (< 1%) but relatively common in the oldest-old (9.1%). Logistic regression modeling showed that in the oldest-old, both intermediate to high ADNC and LATE-NC were independently associated with higher odds of having dementia (OR: 5.09, 95% CI [1.99, 13.06], p < 0.001 for ADNC; OR: 3.28, 95% CI [1.25, 8.57], p = 0.015 for LATE-NC). In the younger-old, by contrast, intermediate to high ADNC and LBD were independently associated with higher odds of having dementia (OR: 4.43, 95% CI [2.27, 8.63], p < 0.001 for ADNC; OR: 2.55, 95% CI [1.21, 5.35], p < 0.014 for LBD), whereas LATE-NC did not show an independent association with dementia. Overall, LATE-NC is strongly associated with arteriolosclerosis and HS in both groups; however, in the younger-old, LATE-NC is associated with other neurodegenerative pathologies, such as ADNC and LBD; whereas in the oldest-old, LATE-NC can exist independent of significant ADNC.
中文翻译:

边缘系统主导的年龄相关 TDP-43 脑病神经病理学改变 (LATE-NC) 的神经病理学关联在最年长的老年人和较年轻的老年人之间存在差异
边缘系统主导的年龄相关 TDP-43 脑病神经病理学改变 (LATE-NC) 最常见于老年人(≥ 90 岁),但也可能出现在较年轻的老年人(< 90 岁)中。在这项研究中,我们比较了 LATE-NC 的神经病理学关联以及 LATE-NC 对最年长老年人和较年轻老年人认知障碍的贡献。我们观察到这两个年龄组中 LATE-NC 的患病率及其与其他并发症的关联存在显着差异。LATE-NC 存在于 30.9% (34/110) 的最年长老年人中,但仅 9.4% (19/203) 存在于较年轻的老年人中。患有 LATE-NC 的年龄最大的参与者更有可能患有海马硬化 (HS)(55.9% vs. 10.5%,p < 0.001)和中度至重度动脉硬化(82.4% vs. 50%,p = 0.007),但不是中度至高度阿尔茨海默病神经病理改变(ADNC)(70.6% vs. 59.2%,p = 0.486)或路易体病(LBD)(20.6% vs. 26.3%,p = 0.793)。 除了海马硬化之外,患有 LATE-NC 的年轻老年人参与者更有可能患有中度至高度 ADNC(94.7% vs. 55.4%,p < 0.001 )和 LBD(63.2% vs. 28.8%,p = 0.013) (42.1% vs. 6.5%,p < 0.001),以及中度至重度动脉硬化(42.1% vs. 15.2%,p = 0.020)。值得注意的是,患有 LATE-NC 和无或低 ADNC 的参与者在较年轻的老年人中非常罕见 (< 1%),但在最年长的老年人中相对常见 (9.1%)。Logistic 回归模型显示,在最年长的老年人中,中度至高度 ADNC 和 LATE-NC 均与患痴呆症的较高几率独立相关(OR:5.09,95% CI [1.99,13.06],ADNC 的 p < 0.001 ;OR:3.28,95% CI [1.25,8.57], 对于 LATE-NC, p = 0.015)。相比之下,在较年轻的老年人中,中度至高度 ADNC 和 LBD 与患痴呆症的较高几率独立相关(OR:4.43,95% CI [2.27,8.63],ADNC p < 0.001;OR: 2.55,95 % CI [1.21,5.35], p LBD < 0.014),而 LATE-NC 并未显示出与痴呆的独立关联。总体而言,LATE-NC 与两组中的动脉硬化和 HS 密切相关;然而,在较年轻的老年人中,LATE-NC 与其他神经退行性疾病相关,例如 ADNC 和 LBD;而在最古老的情况下,LATE-NC 可以独立于显着的 ADNC 存在。



























 京公网安备 11010802027423号
京公网安备 11010802027423号