JACC: Cardiovascular Interventions ( IF 11.3 ) Pub Date : 2021-11-15 , DOI: 10.1016/j.jcin.2021.08.056 Mauro Chiarito 1 , Annapoorna Kini 2 , Anastasios Roumeliotis 2 , Davide Cao 2 , David Power 2 , Samantha Sartori 2 , Adam Reisman 2 , Zhongjie Zhang 2 , Tafadzwa Mtisi 2 , Johny Nicolas 2 , Matteo Nardin 2 , Giulio Stefanini 3 , Usman Baber 4 , Gennaro Giustino 2 , Joseph Sweeny 2 , Roxana Mehran 2 , Samin Sharma 2 , George Dangas 2
|
Objectives
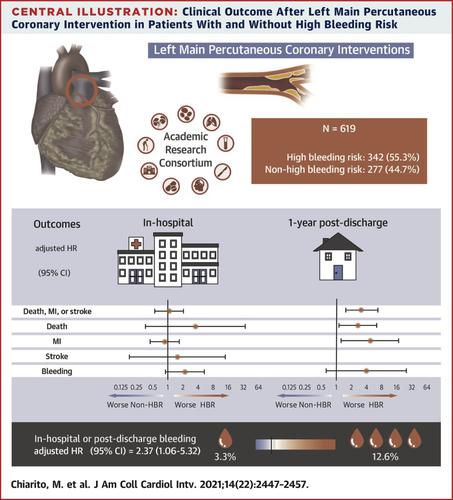
The aim of this study was to determine the prevalence and prognostic impact of high bleeding risk (HBR), as determined by the Academic Research Consortium HBR criteria, in real-world patients undergoing left main (LM) percutaneous coronary intervention (PCI).
Background
LM PCI is often reserved for patients at increased risk for periprocedural adverse events. Patients at HBR represent a relevant percentage of this cohort, but their outcomes after LM PCI are still poorly investigated.
Methods
All patients undergoing LM PCI between 2014 and 2017 at a tertiary care center were prospectively enrolled. Patients were defined as having HBR if they met at least 1 major or 2 minor Academic Research Consortium HBR criteria. The primary endpoint was the composite of all-cause death, myocardial infarction (MI), or stroke at 12 months.
Results
Among 619 enrolled patients, 55.3% were at HBR. The rate of the primary endpoint was 4-fold higher in patients at HBR compared with those without HBR (20.5% vs 4.9%; HR: 4.43; 95% CI: 2.31-8.48), driven by an increased risk for all-cause death (HR: 3.88; 95% CI: 1.88-8.02) and MI (HR: 6.18; 95% CI: 1.83-20.9). Rates of target vessel or lesion revascularization and stent thrombosis were comparable in the 2 groups. Bleeding occurred more frequently in patients at HBR (HR: 3.77; 95% CI: 1.83-7.76). Consistent findings were observed after Cox multivariable regression adjustment.
Conclusions
Among patients undergoing LM PCI, those with HBR are at increased risk for all-cause death, MI, and bleeding. Conversely, rates of repeat revascularization and stent thrombosis were comparable, suggesting frailty and comorbidities as primary causes of worse outcomes in patients at HBR.
中文翻译:

接受左主动脉疾病 PCI 的患者高出血风险的患病率和影响
目标
本研究的目的是确定学术研究联盟 HBR 标准确定的高出血风险 (HBR) 在接受左主干 (LM) 经皮冠状动脉介入治疗 (PCI) 的真实患者中的患病率和预后影响。
背景
LM PCI 通常用于围手术期不良事件风险增加的患者。HBR 的患者占该队列的相关百分比,但他们在 LM PCI 后的结果仍然没有得到很好的研究。
方法
前瞻性招募了 2014 年至 2017 年间在三级医疗中心接受 LM PCI 的所有患者。如果患者满足至少 1 个主要或 2 个次要学术研究联盟 HBR 标准,则他们被定义为患有 HBR。主要终点是 12 个月时全因死亡、心肌梗死 (MI) 或卒中的复合终点。
结果
在 619 名入组患者中,55.3% 在 HBR。由于全因死亡风险增加,HBR 患者的主要终点发生率是未接受 HBR 患者的 4 倍(20.5% 对 4.9%;HR:4.43;95% CI:2.31-8.48) (HR:3.88;95% CI:1.88-8.02)和 MI(HR:6.18;95% CI:1.83-20.9)。两组的靶血管或病变血运重建率和支架内血栓形成率相当。HBR 患者的出血发生率更高(HR:3.77;95% CI:1.83-7.76)。在 Cox 多变量回归调整后观察到一致的结果。
结论
在接受 LM PCI 的患者中,HBR 患者全因死亡、心肌梗死和出血的风险增加。相反,重复血运重建和支架血栓形成的发生率相当,表明虚弱和合并症是 HBR 患者预后较差的主要原因。


























 京公网安备 11010802027423号
京公网安备 11010802027423号