JACC: Heart Failure ( IF 13.0 ) Pub Date : 2021-11-10 , DOI: 10.1016/j.jchf.2021.08.003 Kevin J Clerkin 1 , Oluwafeyijimi Salako 1 , Justin A Fried 1 , Jan M Griffin 1 , Jayant Raikhelkar 1 , Rashmi Jain 1 , Susan Restaino 1 , Paolo C Colombo 1 , Koji Takeda 2 , Maryjane A Farr 1 , Gabriel Sayer 1 , Nir Uriel 1 , Veli K Topkara 1
|
Objectives
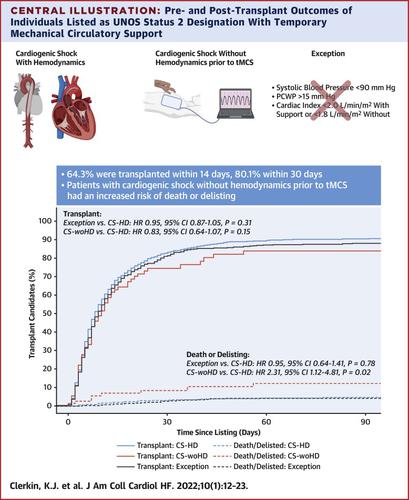
This analysis sought to investigate the waitlist and post-transplant outcomes of individuals bridged to transplantation by using temporary percutaneous endovascular mechanical circulatory support (tMCS) through a status 2 designation (cardiogenic shock and exception).
Background
The 2018 donor heart allocation policy change granted a status 2 designation to patients supported with tMCS.
Methods
Adult patients in the United Network for Organ Sharing registry after October 18, 2018 who received a status 2 designation for tMCS were included and grouped by their status 2 criteria: cardiogenic shock with hemodynamic criteria (CS-HD), cardiogenic shock without hemodynamic criteria before tMCS (CS-woHD), and exception. Baseline characteristics, waitlist events (death and delisting), and post-transplant outcomes were compared.
Results
A total of 2,279 patients met inclusion criteria: 68.6% (n = 1,564) with CS-HD, 3.2% (n = 73) with CS-woHD, and 28.2% (n = 642) with exceptions. A total of 64.2% of patients underwent heart transplantation within 14 days of status 2 listing or upgrade, and 1.9% died or were delisted for worsening clinical condition. Among the 35.8% who did not undergo transplantation following 14 days, only 2.8% went on to receive a left ventricular assist device (LVAD). The 30-day transplantation likelihood was similar among groups: 80.1% for the CS-HD group vs 79.7% for the exception group vs 73.3% for the CS-woHD group; P = 0.31. However, patients who met criteria for CS-woHD had 2.3-fold greater risk of death or delisting (95% CI: 1.10-4.75; P = 0.03) compared with CS-HD patients after multivariable adjustment. Pre-tMCS hemodynamics were not associated with adverse waitlist events.
Conclusions
The use of tMCS is an efficient, safe, and effective strategy as a bridge to transplantation; however, patients with CS-woHD may represent a high-risk cohort. Transition to a durable LVAD was a rare event in this group.
中文翻译:

移植前临时经皮机械循环支持对2018心脏分配系统的影响
目标
该分析旨在调查通过状态 2 指定(心源性休克和异常)使用临时经皮血管内机械循环支持 (tMCS) 桥接到移植的个体的候补名单和移植后结果。
背景
2018 年捐献者心脏分配政策的变化为接受 tMCS 支持的患者授予了状态 2 称号。
方法
2018 年 10 月 18 日之后器官共享联合网络登记处获得 tMCS 状态 2 指定的成年患者被纳入并按其状态 2 标准分组:具有血液动力学标准的心源性休克(CS-HD),之前没有血液动力学标准的心源性休克tMCS (CS-woHD) 和异常。比较了基线特征、候补名单事件(死亡和除名)和移植后结果。
结果
共有 2,279 名患者符合纳入标准:68.6% (n = 1,564) 患有 CS-HD,3.2% (n = 73) 患有 CS-woHD,28.2% (n = 642) 有例外。共有 64.2% 的患者在状态 2 列名或升级后 14 天内接受了心脏移植,1.9% 的患者死亡或因临床状况恶化而被除名。在 14 天后未接受移植的 35.8% 中,只有 2.8% 继续接受左心室辅助装置 (LVAD)。各组之间的 30 天移植可能性相似:CS-HD 组为 80.1%,例外组为 79.7%,CS-woHD 组为 73.3%;P = 0.31。然而,符合 CS-woHD 标准的患者死亡或退市风险增加 2.3 倍(95% CI:1.10-4.75;P =0.03) 与多变量调整后的 CS-HD 患者相比。tMCS 前血流动力学与不良候补事件无关。
结论
使用 tMCS 作为移植的桥梁是一种高效、安全和有效的策略;然而,CS-woHD 患者可能代表高危人群。过渡到耐用的 LVAD 在这个群体中是罕见的事件。



























 京公网安备 11010802027423号
京公网安备 11010802027423号