Journal of Hepatology ( IF 25.7 ) Pub Date : 2021-09-23 , DOI: 10.1016/j.jhep.2021.09.011 Chloé De Broucker 1 , Aurélie Plessier 1 , Isabelle Ollivier-Hourmand 2 , Sébastien Dharancy 3 , Christophe Bureau 4 , Jean-Paul Cervoni 5 , Philippe Sogni 6 , Odile Goria 7 , Olivier Corcos 8 , Riccardo Sartoris 9 , Maxime Ronot 9 , Valérie Vilgrain 9 , Emmanuelle de Raucourt 10 , Kamal Zekrini 1 , Hortense Davy 1 , François Durand 1 , Audrey Payancé 1 , Nadira Fidouh-Houhou 11 , Yazdan Yazdanpanah 12 , Dominique Valla 1 , Pierre-Emmanuel Rautou 1
|
Background & Aims
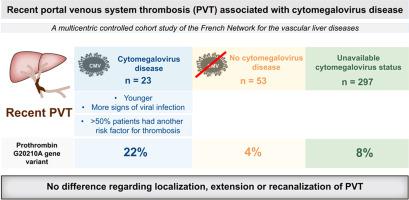
Recent non-malignant non-cirrhotic portal venous system thrombosis (PVT) is a rare condition. Among risk factors for PVT, cytomegalovirus (CMV) disease is usually listed based on a small number of reported cases. The aim of this study was to determine the characteristics and outcomes of PVT associated with CMV disease.
Methods
We conducted a French multicenter retrospective study comparing patients with recent PVT and CMV disease (“CMV positive”; n = 23) to patients with recent PVT for whom CMV testing was negative (“CMV negative”; n = 53) or unavailable (“CMV unknown”; n = 297).
Results
Compared to patients from the “CMV negative” and “CMV unknown” groups, patients from the “CMV positive” group were younger, more frequently had fever, and had higher heart rate, lymphocyte count and serum ALT levels (p ≤0.01 for all). The prevalence of immunosuppression did not differ between the 3 groups (4%, 4% and 6%, respectively). Extension of PVT was similar between the 3 groups. Thirteen out of 23 “CMV positive” patients had another risk factor for thrombosis. Besides CMV disease, the number of risk factors for thrombosis was similar between the 3 groups. Heterozygosity for the prothrombin G20210A gene variant was more frequent in “CMV positive” patients (22%) than in the “CMV negative” (4%, p = 0.01) and “CMV unknown” (8%, p = 0.03) groups. Recanalization rate was not influenced by CMV status.
Conclusions
In patients with recent PVT, features of mononucleosis syndrome should raise suspicion of CMV disease. CMV disease does not influence thrombosis extension nor recanalization. More than half of “CMV positive” patients have another risk factor for thrombosis, with a particular link to the prothrombin G20210A gene variant.
Lay summary
Patients with cytomegalovirus (CMV)-associated portal venous system thrombosis have similar thrombosis extension and evolution as patients without CMV disease. However, patients with CMV-associated portal venous system thrombosis more frequently have the prothrombin G20210A gene variant, suggesting that these entities act synergistically to promote thrombosis.
中文翻译:

近期巨细胞病毒病相关门静脉系统血栓形成的多中心研究
背景与目标
最近的非恶性非肝硬化门静脉系统血栓形成(PVT)是一种罕见的疾病。在 PVT 的危险因素中,巨细胞病毒 (CMV) 疾病通常根据少数报告病例列出。本研究的目的是确定与 CMV 疾病相关的 PVT 的特征和结果。
方法
我们进行了一项法国多中心回顾性研究,比较近期患有 PVT 和 CMV 疾病(“CMV 阳性”;n = 23)的患者与近期患有 CMV 检测阴性(“CMV 阴性”;n = 53)或不可用(“ CMV 未知”;n = 297)。
结果
与“CMV 阴性”和“CMV 未知”组患者相比,“CMV 阳性”组患者更年轻,发热更频繁,心率、淋巴细胞计数和血清 ALT 水平更高(所有p ≤0.01) )。免疫抑制的患病率在 3 组之间没有差异(分别为 4%、4% 和 6%)。PVT 的延长在 3 组之间相似。23 名“CMV 阳性”患者中有 13 名有血栓形成的另一个危险因素。除CMV疾病外,三组之间血栓形成的危险因素数量相似。凝血酶原 G20210A 基因变异的杂合性在“CMV 阳性”患者 (22%) 中比在“CMV 阴性” (4%, p = 0.01) 和“CMV 未知” (8%, p = 0.03) 组。再通率不受 CMV 状态的影响。
结论
在近期有 PVT 的患者中,单核细胞增多症综合征的特征应引起对 CMV 疾病的怀疑。CMV 疾病不影响血栓扩大或再通。超过一半的“CMV 阳性”患者有血栓形成的另一个危险因素,与凝血酶原 G20210A 基因变异有特殊联系。
总结
巨细胞病毒 (CMV) 相关的门静脉系统血栓形成患者与没有 CMV 疾病的患者具有相似的血栓形成延伸和演变。然而,与 CMV 相关的门静脉系统血栓形成患者更常具有凝血酶原 G20210A 基因变异,这表明这些实体协同作用以促进血栓形成。


























 京公网安备 11010802027423号
京公网安备 11010802027423号