当前位置:
X-MOL 学术
›
Brain Pathol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Microvessel stenosis, enlarged perivascular spaces, and fibrinogen deposition are associated with ischemic periventricular white matter hyperintensities
Brain Pathology ( IF 6.4 ) Pub Date : 2021-09-19 , DOI: 10.1111/bpa.13017 Austyn D Roseborough 1 , Berk Rasheed 1 , Youngkyung Jung 2 , Kevin Nishimura 3 , William Pinsky 1 , Kristopher D Langdon 4 , Robert Hammond 5 , Stephen H Pasternak 6 , Ali R Khan 7 , Shawn N Whitehead 1
Brain Pathology ( IF 6.4 ) Pub Date : 2021-09-19 , DOI: 10.1111/bpa.13017 Austyn D Roseborough 1 , Berk Rasheed 1 , Youngkyung Jung 2 , Kevin Nishimura 3 , William Pinsky 1 , Kristopher D Langdon 4 , Robert Hammond 5 , Stephen H Pasternak 6 , Ali R Khan 7 , Shawn N Whitehead 1
Affiliation
|
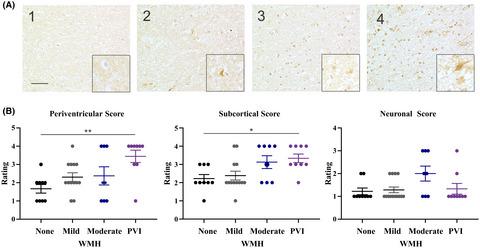
Periventricular white matter hyperintensities (pvWMH) are neuroimaging abnormalities surrounding the lateral ventricles that are apparent on magnetic resonance imaging (MRI). They are associated with age, neurodegenerative disease, and cerebrovascular risk factors. While pvWMH ultimately represent a loss of white matter structural integrity, the pathological causes are heterogeneous in nature, and currently, cannot be distinguished using neuroimaging alone. pvWMH could occur because of a combination of small vessel disease (SVD), ependymal loss, blood–brain barrier dysfunction, and microgliosis. In this study we aimed to characterize microvascular stenosis, fibrinogen extravasation, and microgliosis within pvWMH with and without imaging evidence of periventricular infarction. Using postmortem neuroimaging of human brains (n = 20), we identified pvWMH with and without periventricular infarcts (PVI). We performed histological analysis of microvessel stenosis, perivascular spaces, microgliosis, and immunohistochemistry against fibrinogen as a measure of serum protein extravasation. Herein, we report distinctions between pvWMH with and without periventricular infarcts based on associations with microvessel stenosis, enlarged perivascular spaces, and fibrinogen IHC. Microvessel stenosis was significantly associated with PVI and with cellular deposition of fibrinogen in the white matter. The presence of fibrinogen was associated with PVI and increased number of microglia. These findings suggest that neuroimaging-based detection of infarction within pvWMH may help distinguish more severe lesions, associated with underlying microvascular disease and BBB dysfunction, from milder pvWMH that are a highly frequent finding on MRI.
中文翻译:

微血管狭窄、血管周围空间扩大和纤维蛋白原沉积与缺血性脑室周围白质高信号有关
脑室周围白质高信号 (pvWMH) 是侧脑室周围的神经影像学异常,在磁共振成像 (MRI) 上很明显。它们与年龄、神经退行性疾病和脑血管危险因素有关。虽然 pvWMH 最终代表白质结构完整性的丧失,但病理原因本质上是异质的,目前无法单独使用神经影像学来区分。pvWMH 可能是由小血管疾病 (SVD)、室管膜缺损、血脑屏障功能障碍和小胶质细胞增生共同引起的。在这项研究中,我们旨在描述 pvWMH 内的微血管狭窄、纤维蛋白原外渗和小胶质细胞增生,有无脑室周围梗死的影像学证据。使用人脑的死后神经成像(n = 20),我们确定了有和没有脑室周围梗死 (PVI) 的 pvWMH。我们对微血管狭窄、血管周围间隙、小胶质细胞增生和针对纤维蛋白原的免疫组织化学进行了组织学分析,以衡量血清蛋白外渗。在此,我们根据与微血管狭窄、血管周围间隙扩大和纤维蛋白原 IHC 的相关性报告了 pvWMH 有无脑室周围梗死的区别。微血管狭窄与 PVI 和白质中纤维蛋白原的细胞沉积显着相关。纤维蛋白原的存在与 PVI 和小胶质细胞数量的增加有关。这些发现表明,基于神经影像学的 pvWMH 内梗死检测可能有助于区分与潜在微血管疾病和 BBB 功能障碍相关的更严重的病变,
更新日期:2021-09-19
中文翻译:

微血管狭窄、血管周围空间扩大和纤维蛋白原沉积与缺血性脑室周围白质高信号有关
脑室周围白质高信号 (pvWMH) 是侧脑室周围的神经影像学异常,在磁共振成像 (MRI) 上很明显。它们与年龄、神经退行性疾病和脑血管危险因素有关。虽然 pvWMH 最终代表白质结构完整性的丧失,但病理原因本质上是异质的,目前无法单独使用神经影像学来区分。pvWMH 可能是由小血管疾病 (SVD)、室管膜缺损、血脑屏障功能障碍和小胶质细胞增生共同引起的。在这项研究中,我们旨在描述 pvWMH 内的微血管狭窄、纤维蛋白原外渗和小胶质细胞增生,有无脑室周围梗死的影像学证据。使用人脑的死后神经成像(n = 20),我们确定了有和没有脑室周围梗死 (PVI) 的 pvWMH。我们对微血管狭窄、血管周围间隙、小胶质细胞增生和针对纤维蛋白原的免疫组织化学进行了组织学分析,以衡量血清蛋白外渗。在此,我们根据与微血管狭窄、血管周围间隙扩大和纤维蛋白原 IHC 的相关性报告了 pvWMH 有无脑室周围梗死的区别。微血管狭窄与 PVI 和白质中纤维蛋白原的细胞沉积显着相关。纤维蛋白原的存在与 PVI 和小胶质细胞数量的增加有关。这些发现表明,基于神经影像学的 pvWMH 内梗死检测可能有助于区分与潜在微血管疾病和 BBB 功能障碍相关的更严重的病变,


























 京公网安备 11010802027423号
京公网安备 11010802027423号