The Journal of Thoracic and Cardiovascular Surgery ( IF 6 ) Pub Date : 2021-09-08 , DOI: 10.1016/j.jtcvs.2021.08.075 Wen-Lun Wang, I-Wei Chang, Sin-Hua Moi, Ming-Hung Hsu, Chi-Jen Chen, Chao-Tien Hsu, Hsiu-Po Wang, Ching-Tai Lee
|
Background
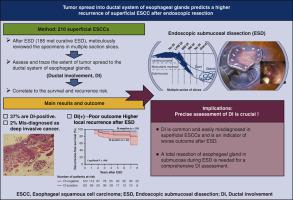
Endoscopic submucosal dissection (ESD) has become the standard treatment for superficial esophageal squamous cell neoplasia (SESCN); however, local recurrence still occurs occasionally even in patients who meet the current curative criteria. Esophageal ducts of the submucosal gland may serve as a pathway for the spread of SESCN to a deeper layer. However, the clinical impact of ductal involvement (DI) in patients undergoing ESD has yet to be investigated.
Methods
We consecutively enrolled patients with SESCN who were treated with ESD. The resected specimens were meticulously reviewed in multiple section slices for the presence and resected margins of DI, and their correlations with clinical factors were evaluated.
Results
A total of 210 lesions were analyzed, of which 78 (37.1%) presented with DI. The presence of submucosal invasion, lymphovascular invasion (LVI), and DI were indicators of worse prognosis (P < .05). Deep extended DIs were misdiagnosed as deep submucosal invasive cancer in 4 cases (2%). Of the 185 patients who met the criteria for curative ESD (ie, R0 resection and no deep submucosal invasion or LVI), 11 (5.9%) developed local recurrence/metastasis during a mean follow-up of 55.2 months (range, 6 to 140) months. Compared with patients with without DI, patients with DI had worse recurrence-free survival (P = .008, log-rank test) and a higher local risk of recurrence (12.7% vs 2.5%) after curative ESD (hazard ratio, 4.20; P = .038).
Conclusions
A precise histological assessment of DI in SESCN is crucial after ESD, given that DI is common and associated with worse outcome. Whether total removal of esophageal glands/ducts can improve outcome requires future study.
中文翻译:

浅表食管鳞状细胞瘤患者黏膜下腺导管系统肿瘤扩散的评估:内镜下切除的意义
背景
内镜黏膜下剥离术(ESD)已成为食管浅表鳞状细胞瘤(SESCN)的标准治疗方法;然而,即使在符合当前治愈标准的患者中,仍偶尔会发生局部复发。黏膜下腺的食管导管可作为 SECN 向更深层扩散的途径。然而,导管受累 (DI) 对接受 ESD 的患者的临床影响尚待研究。
方法
我们连续招募了接受 ESD 治疗的 SECN 患者。对切除的标本在多个切片切片中仔细审查DI的存在和切除边缘,并评估其与临床因素的相关性。
结果
共分析了 210 个病灶,其中 78 个(37.1%)出现 DI。黏膜下浸润、淋巴血管浸润 (LVI) 和 DI 是预后较差的指标 ( P < .05)。4 例(2%)深扩展 DI 被误诊为深部黏膜下浸润癌。在 185 名符合治愈性 ESD 标准(即 R0 切除且无深部粘膜下浸润或 LVI)的患者中,11 名(5.9%)在平均 55.2 个月(范围,6 至 140 ) 个月。与没有 DI 的患者相比,有 DI 的患者在治愈性 ESD 后的无复发生存期更差(P = .008,对数秩检验)和更高的局部复发风险(12.7% vs 2.5%)(风险比,4.20;P = .038)。
结论
考虑到 DI 很常见并且与更差的结果相关,在 ESD 后对 SECN 中的 DI 进行精确的组织学评估至关重要。完全切除食管腺/导管是否可以改善结果需要未来的研究。



























 京公网安备 11010802027423号
京公网安备 11010802027423号