Journal of Allergy and Clinical Immunology ( IF 14.2 ) Pub Date : 2021-08-20 , DOI: 10.1016/j.jaci.2021.08.007 Allyson Mateja 1 , Qinlu Wang 2 , Jack Chovanec 3 , Jiwon Kim 3 , Kenneth J Wilson 4 , Lawrence B Schwartz 5 , Sarah C Glover 6 , Melody C Carter 3 , Dean D Metcalfe 3 , Erica Brittain 7 , Jonathan J Lyons 3
|
Background
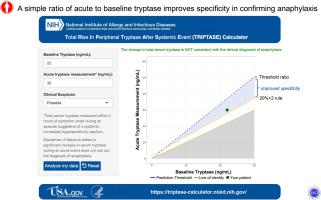
Acute increases of ≥20% + 2 ng/mL (20 + 2 rule) over basal serum tryptase (BST) is the recommended threshold supporting a clinical diagnosis of anaphylaxis. Prospective studies have demonstrated high sensitivity for this algorithm after parenteral exposure, but specificity has not been evaluated.
Objective
We sought to define a serum tryptase change that distinguishes baseline variability from anaphylaxis on the basis of intraindividual variation in BST.
Methods
Ninety-three total subjects with atopy (n = 62) or hereditary α-tryptasemia (HαT) (n = 31) and ≥2 BST measurements were identified. Sequential BST variability measurements were modeled and threshold ratios that optimized sensitivity and/or specificity determined. Models were tested in 22 individuals with physician-diagnosed anaphylaxis and validated in independent cohorts of individuals with HαT (n = 33), indolent systemic mastocytosis (ISM) (n = 52), and ISM + HαT (n = 12). Mature tryptase levels were measured in HαT (n = 19) and ISM (n = 20). An online application was developed for clinical use.
Results
As a result of BST variability, 9.7% (9/93) of primary cohort patients, and 18% (6/33) of HαT, 30% (16/53) of ISM, and 25% (3/12) of ISM + HαT patients from validation cohorts met the 20 + 2 rule despite absent immediate hypersensitivity symptoms; mature tryptase was noncontributory among individuals with HαT or ISM at baseline. A ratio of acute tryptase/BST exceeding 1.685 provided the optimized diagnostic rule for jointly maximizing sensitivity and specificity. Statistically significant improvement in specificity relative to the 20 + 2 rule was observed among individuals with elevated BST caused by HαT and ISM.
Conclusions
Using an acute tryptase/BST ratio of 1.685 improves specificity of measured changes among individuals with HαT and ISM while maintaining high sensitivity for confirmation of anaphylaxis.
中文翻译:

定义血清类胰蛋白酶水平的基线变异性可提高识别过敏反应的准确性
背景
超过基础血清类胰蛋白酶 (BST) 的急性增加 ≥ 20% + 2 ng/mL(20 + 2 规则)是支持过敏反应临床诊断的推荐阈值。前瞻性研究表明,该算法在肠胃外暴露后具有高敏感性,但尚未评估特异性。
客观的
我们试图定义一种血清类胰蛋白酶变化,它根据 BST 的个体内变异来区分基线变异和过敏反应。
方法
确定了 93 名患有特应性 (n = 62) 或遗传性 α-类胰酶血症 (HαT) (n = 31) 且 BST 测量值≥2 的受试者。对顺序 BST 变异性测量进行建模,并确定优化灵敏度和/或特异性的阈值比率。模型在 22 名经医生诊断为过敏反应的个体中进行了测试,并在患有 HαT (n = 33)、惰性系统性肥大细胞增多症 (ISM) (n = 52) 和 ISM + HαT (n = 12) 的独立队列中进行了验证。在 HαT (n = 19) 和 ISM (n = 20) 中测量了成熟的类胰蛋白酶水平。开发了一个在线应用程序供临床使用。
结果
由于 BST 变异性,9.7% (9/93) 的主要队列患者、18% (6/33) 的 HαT、30% (16/53) 的 ISM 和 25% (3/12) 的 ISM + 来自验证队列的 HαT 患者满足 20 + 2 规则,尽管没有立即超敏反应症状;成熟的类胰蛋白酶在基线时具有 HαT 或 ISM 的个体中没有作用。急性类胰蛋白酶/BST 的比率超过 1.685 提供了优化的诊断规则,以共同最大化灵敏度和特异性。在由 HαT 和 ISM 引起的 BST 升高的个体中观察到相对于 20 + 2 规则的特异性在统计学上有显着改善。
结论
使用 1.685 的急性类胰蛋白酶/BST 比率可提高 HαT 和 ISM 患者测量变化的特异性,同时保持确认过敏反应的高灵敏度。



























 京公网安备 11010802027423号
京公网安备 11010802027423号