The Journal of Thoracic and Cardiovascular Surgery ( IF 6 ) Pub Date : 2021-08-20 , DOI: 10.1016/j.jtcvs.2021.08.033 Akiko Tanaka 1 , Hung Nguyen 1 , Jaydeep S Dhillon 1 , Masaki Nakamura 1 , Shao-Feng Zhou 2 , Harleen K Sandhu 1 , Charles C Miller 1 , Hazim J Safi 1 , Anthony L Estrera 1
|
Objective
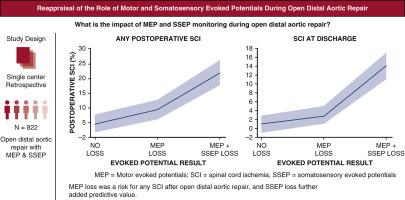
Intraoperative motor and somatosensory evoked potentials have been applied to monitor spinal cord ischemia during repair. However, their predictive values remain controversial. The purpose of this study was to evaluate the impact of motor evoked potentials and somatosensory evoked potentials on spinal cord ischemia during open distal aortic repair.
Methods
Our group began routine use of both somatosensory evoked potentials and motor evoked potentials at the end of 2004. This study used a historical cohort design, using risk factor and outcome data from our department's prospective registry. Univariate and multivariable statistics for risk-adjusted effects of motor evoked potentials and somatosensory evoked potentials on neurologic outcome and model discrimination were assessed with receiver operating characteristic curves.
Results
Both somatosensory evoked potentials and motor evoked potentials were measured in 822 patients undergoing open distal aortic repair between December 2004 and December 2019. Both motor evoked potentials and somatosensory evoked potentials were intact for the duration of surgery in 348 patients (42%). Isolated motor evoked potential loss was observed in 283 patients (34%), isolated somatosensory evoked potential loss was observed in 18 patients (3%), and both motor evoked potential and somatosensory evoked potential loss were observed in 173 patients (21%). No spinal cord ischemia occurred in the 18 cases with isolated somatosensory evoked potential loss. When both signals were lost, signal loss happened in the order of motor evoked potentials and then somatosensory evoked potentials. Immediate spinal cord ischemia occurred in none of those without signal loss, 4 of 283 (1%) with isolated motor evoked potential loss, and 15 of 173 (9%) with motor evoked potential plus somatosensory evoked potential loss. Delayed spinal cord ischemia occurred in 12 of 348 patients (3%) with intact evoked potentials, 24 of 283 patients (8%) with isolated motor evoked potentials loss, and 27 of 173 patients (15%) with motor evoked potentials + somatosensory evoked potentials loss (P < .001). Motor evoked potentials and somatosensory evoked potentials loss were each independently associated with spinal cord ischemia. For immediate spinal cord ischemia, no return of motor evoked potential signals at the conclusion of the surgery had the highest odds ratio of 15.87, with a receiver operating characteristic area under the curve of 0.936, whereas motor evoked potential loss had the highest odds ratio of 3.72 with an area under the curve of 0.638 for delayed spinal cord ischemia.
Conclusions
Somatosensory evoked potentials and motor evoked potentials are both important monitoring measures to predict and prevent spinal cord ischemia during and after open distal aortic repairs. Intraoperative motor evoked potential loss is a risk for immediate and delayed spinal cord ischemia after open distal aortic repair, and somatosensory evoked potential loss further adds predictive value to the motor evoked potential.
中文翻译:

重新评估开放性远端主动脉修复过程中运动和体感诱发电位的作用
客观的
术中运动和体感诱发电位已用于监测修复过程中的脊髓缺血。然而,它们的预测价值仍然存在争议。本研究的目的是评估运动诱发电位和体感诱发电位对开放性远端主动脉修复期间脊髓缺血的影响。
方法
我们小组于 2004 年底开始常规使用体感诱发电位和运动诱发电位。这项研究采用历史队列设计,使用来自我们部门前瞻性登记的风险因素和结果数据。使用接受者操作特征曲线评估运动诱发电位和体感诱发电位对神经系统结果和模型辨别的风险调整影响的单变量和多变量统计数据。
结果
2004 年 12 月至 2019 年 12 月期间,测量了 822 名接受开放性远端主动脉修复术的患者的体感诱发电位和运动诱发电位。348 名患者 (42%) 的运动诱发电位和体感诱发电位在手术期间保持完整。283 名患者(34%)观察到孤立运动诱发电位丧失,18 名患者(3%)观察到孤立体感诱发电位丧失,173 名患者(21%)同时观察到运动诱发电位和体感诱发电位丧失。18例孤立性体感诱发电位丧失者均未发生脊髓缺血。当两个信号都丢失时,信号丢失的顺序依次为运动诱发电位、体感诱发电位。没有信号丢失的患者中没有立即发生脊髓缺血,283 名有孤立运动诱发电位丢失的患者中有 4 名(1%)发生脊髓缺血,173 名有运动诱发电位加体感诱发电位丢失的患者中有 15 名(9%)发生立即脊髓缺血。348 名诱发电位完整的患者中,有 12 名(3%)发生迟发性脊髓缺血;283 名孤立运动诱发电位丧失的患者中,有 24 名(8%)发生迟发性脊髓缺血;173 名运动诱发电位 + 体感诱发电位丧失的患者中,有 27 名(15%)发生迟发性脊髓缺血。潜在损失 ( P < .001)。运动诱发电位和体感诱发电位损失均与脊髓缺血独立相关。对于立即脊髓缺血,手术结束时运动诱发电位信号没有返回的比值比最高为 15.87,曲线下接收者操作特征面积为 0.936,而运动诱发电位丢失的比值比最高为延迟性脊髓缺血的曲线下面积为 3.72,曲线下面积为 0.638。
结论
体感诱发电位和运动诱发电位都是预测和预防开放性远端主动脉修复期间和之后脊髓缺血的重要监测措施。术中运动诱发电位丧失是开放性远端主动脉修复术后立即和迟发性脊髓缺血的风险,体感诱发电位丧失进一步增加了运动诱发电位的预测价值。



























 京公网安备 11010802027423号
京公网安备 11010802027423号