Current HIV Research ( IF 1 ) Pub Date : 2021-11-30 , DOI: 10.2174/1570162x19666210805092258 Sumedha Chhatre 1 , George Woody 1 , David S Metzger 1 , Ravishankar Jayadevappa 2
|
Background: Improved survivorship among persons living with HIV translates into a higher risk of medical comorbidities.
Objectives: We assessed the association between the intersection of physical (HIV) and mental health (psychiatric) conditions and intermediate outcomes.
Methods: This was a cross-sectional study of the Medical Expenditure Panel Survey (MEPS)- Household Component between 1996 and 2016. We created four groups for persons aged ≥18: (1) HIV + psychiatric comorbidity, (2) HIV, (3) psychiatric comorbidity, and (4) no-HIV/no-psychiatric comorbidity. We compared the burden of medical comorbidities (metabolic disorders, cardiovascular disease, cancers, infectious diseases, pain, and substance use) among groups using chisquare tests. We used logistic regression to determine the association between group status and medical comorbidity.
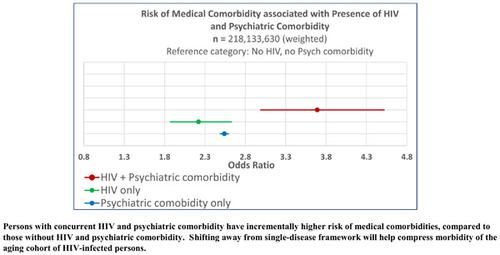
Results: Of 218,133,630 (weighted) persons aged ≥18, 0.18% were HIV-positive. Forty-three percent of the HIV group and 19% of the no-HIV group had psychiatric comorbidities. Half of the HIV+ psychiatric disorder group had at least one medical comorbidity. Compared to the no- HIV/no-psychiatric comorbidity group, the HIV + psychiatric comorbidity group had the highest odds of medical comorbidity (OR= 3.69, 95% CI = 2.99, 4.52).
Conclusion: Persons presenting with HIV + psychiatric comorbidity had higher odds of medical comorbidities of pain, cancer, cardiovascular disease, substance use, metabolic disorders and infectious diseases, beyond that experienced by persons with HIV infection or psychiatric disorders, independently. Future research will focus on the mediating effects of social determinants and biological factors on outcomes such as the quality of life, cost and mortality. This will facilitate a shift away from the single-disease framework and compress morbidity of the aging cohort of HIV-infected persons.
中文翻译:

艾滋病毒/艾滋病和精神病合并症患者的慢性病负担
背景:艾滋病病毒感染者生存率的提高转化为合并症的风险更高。
目标:我们评估了身体 (HIV) 和心理健康 (精神) 状况与中间结果之间的关联。
方法:这是一项对 1996 年至 2016 年间医疗支出小组调查 (MEPS) - 家庭部分的横断面研究。我们为 18 岁以上的人创建了四个组:(1) HIV + 精神疾病,(2) HIV,( 3) 精神病合并症,和 (4) 无 HIV/无精神病合并症。我们使用卡方检验比较了各组医学合并症(代谢紊乱、心血管疾病、癌症、传染病、疼痛和物质使用)的负担。我们使用逻辑回归来确定群体状态与内科合并症之间的关联。
结果:在 218,133,630(加权)年龄≥18 岁的人中,0.18% 为 HIV 阳性。43% 的 HIV 组和 19% 的非 HIV 组有精神疾病。一半的 HIV+ 精神疾病组有至少一种合并症。与无 HIV/无精神病合并症组相比,HIV + 精神病合并症组发生内科合并症的几率最高(OR= 3.69, 95% CI = 2.99, 4.52)。
结论:与 HIV 感染者或精神疾病患者相比,患有 HIV + 精神疾病的人出现疼痛、癌症、心血管疾病、物质使用、代谢紊乱和传染病等医学合并症的几率更高。未来的研究将侧重于社会决定因素和生物因素对生活质量、成本和死亡率等结果的中介作用。这将有助于摆脱单一疾病框架,并降低艾滋病毒感染者老龄化人群的发病率。


























 京公网安备 11010802027423号
京公网安备 11010802027423号