Brain Research ( IF 2.9 ) Pub Date : 2021-07-22 , DOI: 10.1016/j.brainres.2021.147584 Quanlei Liu 1 , Changkai Hou 2 , Hao Zhang 1 , Cong Fu 1 , Weihan Wang 1 , Bangyue Wang 2 , Jian Li 2 , Yan Zhao 2 , Xinyu Yang 2
|
Background and purpose
Blood that enters the subarachnoid space (SAS) and its breakdown products are neurotoxic and are the principal inducers of brain injury after subarachnoid hemorrhage (SAH). Recently, meningeal lymphatic vessels (MLVs) have been proven to play an important role in clearing erythrocytes that arise from SAH, as well as other macromolecular solutes. However, evidence demonstrating the relationship between MLVs and brain injury after SAH is still limited. Therefore, we performed this study to observe the effects of meningeal lymphatic impairment on early brain injury (EBI) after experimental SAH.
Methods
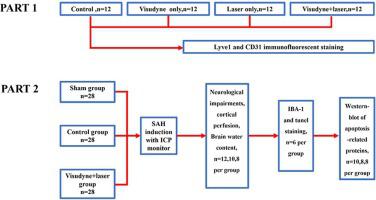
The MLVs of C57BL/6 male adult mice were ablated by injecting Visudyne into the cisterna magna and transcranially photoconverting it with laser light. The MLVs were then examined by immunofluorescence staining for lyve-1. Next, both the MLV-ablated group and the control group (normal mice) underwent filament perforation to model SAH or sham operation. We assessed the cortical perfusion of all the mice before SAH induction, 5 min after SAH and 24 h after SAH. In addition, we evaluated neurological function deficits by Garcia scores and measured brain water content at 24 h post SAH. Then, neuroinflammation and neural apoptosis in the mouse brain were also examined.
Results
Visudyne and transcranial photoconversion treatment notably ablated mouse MLVs. Five minutes after SAH induction, cortical perfusion was significantly impaired, and after 24 h, this impairment was ameliorated considerably in the control group but ameliorated only slightly or worsened in the MLV-ablated group. Additionally, the MLVablated group presented worse neurological function deficits and more severe brain edema than the control group. More notably, neuroinflammation and neural apoptosis were also observed.
Conclusion
Ablation of MLVs by Visudyne treatment exacerbated EBI after experimental SAH in mice. The worsening of EBI may have arisen from limited drainage of blood and other breakdown products, which are thought to cause brain edema, neuroinflammation, neuronal apoptosis and other pathological processes.
中文翻译:

实验性蛛网膜下腔出血后脑膜淋巴管受损加重早期脑损伤
背景和目的
进入蛛网膜下腔 (SAS) 的血液及其分解产物具有神经毒性,是蛛网膜下腔出血 (SAH) 后脑损伤的主要诱因。最近,脑膜淋巴管 (MLV) 已被证明在清除由 SAH 产生的红细胞以及其他大分子溶质中起重要作用。然而,证明 MLV 与 SAH 后脑损伤之间关系的证据仍然有限。因此,我们进行了这项研究,以观察脑膜淋巴损伤对实验性 SAH 后早期脑损伤 (EBI) 的影响。
方法
C57BL/6 雄性成年小鼠的 MLV 通过将 Visudyne 注射到小脑池中并用激光对其进行经颅光转换来消融。然后通过 lyve-1 的免疫荧光染色检查 MLV。接下来,MLV 消融组和对照组(正常小鼠)均进行细丝穿孔以模拟 SAH 或假手术。我们在 SAH 诱导前、SAH 后 5 分钟和 SAH 后 24 小时评估了所有小鼠的皮质灌注。此外,我们通过 Garcia 评分评估了神经功能缺陷,并在 SAH 后 24 小时测量了脑含水量。然后,还检查了小鼠大脑中的神经炎症和神经细胞凋亡。
结果
Visudyne 和经颅光转换治疗显着消融了小鼠 MLV。SAH 诱导后 5 分钟,皮质灌注显着受损,24 小时后,对照组的这种损伤显着改善,但在 MLV 消融组中仅轻微改善或恶化。此外,与对照组相比,MLVablated 组表现出更严重的神经功能缺陷和更严重的脑水肿。更值得注意的是,还观察到神经炎症和神经细胞凋亡。
结论
Visudyne 治疗对 MLVs 的消融加剧了小鼠实验性 SAH 后的 EBI。EBI 的恶化可能源于血液和其他分解产物的排出受限,这些产物被认为会导致脑水肿、神经炎症、神经元凋亡和其他病理过程。


























 京公网安备 11010802027423号
京公网安备 11010802027423号