当前位置:
X-MOL 学术
›
Stem Cells Transl. Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Type 2 diabetes mellitus duration and obesity alter the efficacy of autologously transplanted bone marrow-derived mesenchymal stem/stromal cells
STEM CELLS Translational Medicine ( IF 6 ) Pub Date : 2021-06-03 , DOI: 10.1002/sctm.20-0506 Liem Thanh Nguyen 1 , Duc M Hoang 1 , Kien T Nguyen 1 , Duc M Bui 2 , Hieu T Nguyen 1 , Hong T A Le 1 , Van T Hoang 1 , Hue T H Bui 3 , Phuong T M Dam 3 , Xuan T A Hoang 1 , Anh T L Ngo 1 , Hang M Le 3 , Nhi Y Phung 3 , Duc M Vu 1 , Trung T Duong 1 , Tu D Nguyen 3 , Lien T Ha 4 , Hoa T P Bui 4 , Hoa K Nguyen 1 , Michael Heke 5 , Anh V Bui 3
STEM CELLS Translational Medicine ( IF 6 ) Pub Date : 2021-06-03 , DOI: 10.1002/sctm.20-0506 Liem Thanh Nguyen 1 , Duc M Hoang 1 , Kien T Nguyen 1 , Duc M Bui 2 , Hieu T Nguyen 1 , Hong T A Le 1 , Van T Hoang 1 , Hue T H Bui 3 , Phuong T M Dam 3 , Xuan T A Hoang 1 , Anh T L Ngo 1 , Hang M Le 3 , Nhi Y Phung 3 , Duc M Vu 1 , Trung T Duong 1 , Tu D Nguyen 3 , Lien T Ha 4 , Hoa T P Bui 4 , Hoa K Nguyen 1 , Michael Heke 5 , Anh V Bui 3
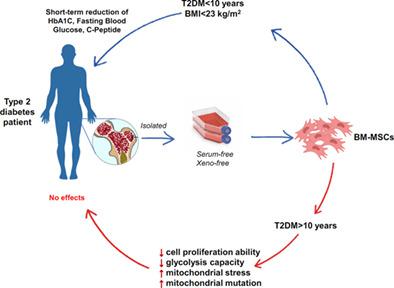
Affiliation
|
Human bone marrow-derived mesenchymal stem/stromal cells (BM-MSCs) represent promising stem cell therapy for the treatment of type 2 diabetes mellitus (T2DM), but the results of autologous BM-MSC administration in T2DM patients are contradictory. The purpose of this study was to test the hypothesis that autologous BM-MSC administration in T2DM patient is safe and that the efficacy of the treatment is dependant on the quality of the autologous BM-MSC population and administration routes. T2DM patients were enrolled, randomly assigned (1:1) by a computer-based system into the intravenous and dorsal pancreatic arterial groups. The safety was assessed in all the treated patients, and the efficacy was evaluated based on the absolute changes in the hemoglobin A1c, fasting blood glucose, and C-peptide levels throughout the 12-month follow-up. Our data indicated that autologous BM-MSC administration was well tolerated in 30 T2DM patients. Short-term therapeutic effects were observed in patients with T2DM duration of <10 years and a body mass index <23, which is in line with the phenotypic analysis of the autologous BM-MSC population. T2DM duration directly altered the proliferation rate of BM-MSCs, abrogated the glycolysis and mitochondria respiration of BM-MSCs, and induced the accumulation of mitochondria DNA mutation. Our data suggest that autologous administration of BM-MSCs in the treatment of T2DM should be performed in patients with T2DM duration <10 years and no obesity. Prior to further confirming the effects of T2DM on BM-MSC biology, future work with a larger cohort focusing on patients with different T2DM history is needed to understand the mechanism underlying our observation.
中文翻译:

2型糖尿病病程和肥胖改变自体移植骨髓间充质干/基质细胞的功效
人骨髓来源的间充质干/基质细胞 (BM-MSCs) 代表了治疗 2 型糖尿病 (T2DM) 的有希望的干细胞疗法,但自体 BM-MSC 在 T2DM 患者中给药的结果是矛盾的。本研究的目的是验证 T2DM 患者中自体 BM-MSC 给药是安全的假设,并且治疗效果取决于自体 BM-MSC 群的质量和给药途径。T2DM 患者被纳入,通过基于计算机的系统随机分配 (1:1) 到静脉内和背侧胰腺动脉组。在所有接受治疗的患者中评估了安全性,并根据整个 12 个月随访期间血红蛋白 A1c、空腹血糖和 C 肽水平的绝对变化来评估疗效。我们的数据表明,自体 BM-MSC 给药在 30 名 T2DM 患者中具有良好的耐受性。在T2DM病程<10年且体重指数<23的患者中观察到短期治疗效果,这与自体BM-MSC群体的表型分析一致。T2DM 持续时间直接改变 BM-MSCs 的增殖速率,消除 BM-MSCs 的糖酵解和线粒体呼吸,并诱导线粒体 DNA 突变的积累。我们的数据表明,对于 T2DM 病程 <10 年且无肥胖症的患者,应在 T2DM 治疗中进行自体 BM-MSCs 给药。在进一步确认 T2DM 对 BM-MSC 生物学的影响之前,
更新日期:2021-06-03
中文翻译:

2型糖尿病病程和肥胖改变自体移植骨髓间充质干/基质细胞的功效
人骨髓来源的间充质干/基质细胞 (BM-MSCs) 代表了治疗 2 型糖尿病 (T2DM) 的有希望的干细胞疗法,但自体 BM-MSC 在 T2DM 患者中给药的结果是矛盾的。本研究的目的是验证 T2DM 患者中自体 BM-MSC 给药是安全的假设,并且治疗效果取决于自体 BM-MSC 群的质量和给药途径。T2DM 患者被纳入,通过基于计算机的系统随机分配 (1:1) 到静脉内和背侧胰腺动脉组。在所有接受治疗的患者中评估了安全性,并根据整个 12 个月随访期间血红蛋白 A1c、空腹血糖和 C 肽水平的绝对变化来评估疗效。我们的数据表明,自体 BM-MSC 给药在 30 名 T2DM 患者中具有良好的耐受性。在T2DM病程<10年且体重指数<23的患者中观察到短期治疗效果,这与自体BM-MSC群体的表型分析一致。T2DM 持续时间直接改变 BM-MSCs 的增殖速率,消除 BM-MSCs 的糖酵解和线粒体呼吸,并诱导线粒体 DNA 突变的积累。我们的数据表明,对于 T2DM 病程 <10 年且无肥胖症的患者,应在 T2DM 治疗中进行自体 BM-MSCs 给药。在进一步确认 T2DM 对 BM-MSC 生物学的影响之前,



























 京公网安备 11010802027423号
京公网安备 11010802027423号