Journal of the American Society of Echocardiography ( IF 6.5 ) Pub Date : 2021-05-31 , DOI: 10.1016/j.echo.2021.05.016 Alexandros Papachristidis 1 , Sandro Queirós 2 , Konstantinos C Theodoropoulos 3 , Jan D'hooge 4 , Patrick Rafter 5 , Giovanni Masoero 3 , Spyridon Zidros 3 , Gianpiero Pagnano 3 , Marilou Huang 3 , Luke Dancy 1 , Daniel Sado 1 , Ajay M Shah 1 , Francis D Murgatroyd 1 , Mark J Monaghan 1
|
Background
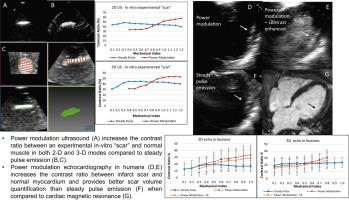
Myocardial scar appears brighter compared with normal myocardium on echocardiography because of differences in tissue characteristics. The aim of this study was to test how different ultrasound pulse characteristics affect the brightness contrast (i.e., contrast ratio [CR]) between tissues of different acoustic properties, as well as the accuracy of assessing tissue volume.
Methods
An experimental in vitro “scar” model was created using overheated and raw pieces of commercially available bovine muscle. Two-dimensional and three-dimensional ultrasound scanning of the model was performed using combinations of ultrasound pulse characteristics: ultrasound frequency, harmonics, pulse amplitude, steady pulse (SP) emission, power modulation (PM), and pulse inversion modalities.
Results
On both two-dimensional and three-dimensional imaging, the CR between the “scar” and its adjacent tissue was higher when PM was used. PM, as well as SP ultrasound imaging, provided good “scar” volume quantification. When tested on 10 “scars” of different size and shape, PM resulted in lower bias (−9.7 vs 54.2 mm3) and narrower limits of agreement (−168.6 to 149.2 mm3 vs −296.0 to 404.4 mm3, P = .03). The interobserver variability for “scar” volume was better with PM (intraclass correlation coefficient = 0.901 vs 0.815). Two-dimensional and three-dimensional echocardiography with PM and SP was performed on 15 individuals with myocardial scar secondary to infarction. The CR was higher on PM imaging. Using cardiac magnetic resonance as a reference, quantification of myocardial scar volume showed better agreement when PM was used (bias, −645 mm3; limits of agreement, −3,158 to 1,868 mm3) as opposed to SP (bias, −1,138 mm3; limits of agreement, −5,510 to 3,233 mm3).
Conclusions
The PM modality increased the CR between tissues with different acoustic properties in an experimental in vitro “scar” model while allowing accurate quantification of “scar” volume. By applying the in vitro findings to humans, PM resulted in higher CR between scarred and healthy myocardium, providing better scar volume quantification than SP compared with cardiac magnetic resonance.
中文翻译:

供应商特定超声波束形成和处理技术对体外实验“疤痕”可视化的影响:二维和三维超声心动图对心肌疤痕成像的影响
背景
由于组织特征的差异,心肌瘢痕在超声心动图上与正常心肌相比显得更亮。本研究的目的是测试不同的超声脉冲特性如何影响不同声学特性的组织之间的亮度对比度(即对比度[CR]),以及评估组织体积的准确性。
方法
一个实验性的体外“疤痕”模型是使用商业上可买到的过热和原始的牛肌肉块创建的。使用超声脉冲特征的组合对模型进行二维和三维超声扫描:超声频率、谐波、脉冲幅度、稳定脉冲 (SP) 发射、功率调制 (PM) 和脉冲反转方式。
结果
在二维和三维成像中,使用 PM 时“疤痕”与其相邻组织之间的 CR 较高。PM 以及 SP 超声成像提供了良好的“疤痕”体积量化。在对 10 个不同大小和形状的“疤痕”进行测试时,PM 导致偏差较低(-9.7 对 54.2 mm 3)和更窄的一致性限制(-168.6 至 149.2 mm 3对 -296.0 至 404.4 mm 3,P = .03)。“疤痕”体积的观察者间变异性与 PM 相比更好(组内相关系数 = 0.901 vs 0.815)。对 15 名继发于梗塞的心肌瘢痕患者进行了 PM 和 SP 的二维和三维超声心动图检查。PM 成像的 CR 较高。使用心脏磁共振作为参考,与 SP(偏差,-1,138 mm 3)相比,使用 PM(偏差,-645 mm 3 ;协议限制,-3,158 至 1,868 mm 3 )时,心肌瘢痕体积的量化显示出更好的一致性; 协议限制,-5,510 至 3,233 mm 3 )。
结论
PM 模式在实验性体外“疤痕”模型中增加了具有不同声学特性的组织之间的 CR,同时允许准确量化“疤痕”体积。通过将体外研究结果应用于人类,PM 导致疤痕和健康心肌之间的 CR 更高,与心脏磁共振相比,提供了比 SP 更好的疤痕体积量化。


























 京公网安备 11010802027423号
京公网安备 11010802027423号