Current Neuropharmacology ( IF 5.3 ) Pub Date : 2021-07-31 , DOI: 10.2174/1570159x19666210125153308 Jacek M Kwiecien 1
|
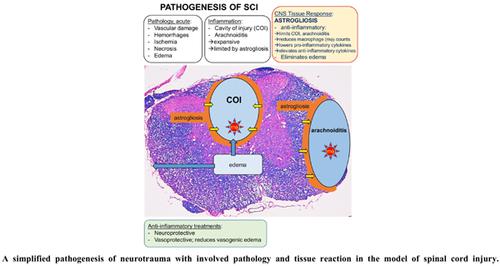
The spinal cord injury (SCI) initiates an extraordinarily protracted disease with 3 phases; acute, inflammatory, and resolution that are restricted to the cavity of injury (COI) or arachnoiditis by a unique CNS reaction against the severity of destructive inflammation. While the severity of inflammation involving the white matter is fueled by a potently immunogenic activity of damaged myelin, its sequestration in the COI and its continuity with the cerebrospinal fluid of the subdural space allow anti-inflammatory therapeutics infused subdurally to inhibit phagocytic macrophage infiltration and thus provide neuroprotection. The role of astrogliosis in containing and ultimately in eliminating severe destructive inflammation post-trauma appears obvious but is not yet sufficiently understood to use in therapeutic neuroprotective and neuroregenerative strategies. An apparent antiinflammatory activity of reactive astrocytes is paralleled by their active role in removing excess edema fluid in blood-brain barrier damaged by inflammation. Recently elucidated pathogenesis of neurotrauma, including SCI, traumatic brain injury (TBI), and stroke, calls for the following principal therapeutic steps in its treatment leading to the recovery of neurologic function: (1) inhibition and elimination of destructive inflammation from the COI with accompanying reduction of vasogenic edema, (2) insertion into the COI of a functional bridge supporting the crossing of regenerating axons, (3) enabling regeneration of axons to their original synaptic targets by temporary safe removal of myelin in targeted areas of white matter, (4) in vivo, systematic monitoring of the consecutive therapeutic steps. The focus of this paper is on therapeutic step 1.
中文翻译:

神经创伤的发病机制表明了神经保护治疗的目标
脊髓损伤 (SCI) 引发一种极其持久的疾病,分为 3 个阶段;急性、炎症和消退仅限于损伤腔 (COI) 或蛛网膜炎,通过独特的中枢神经系统反应对抗破坏性炎症的严重程度。虽然涉及白质的炎症的严重性是由受损髓磷脂的强免疫原性活性加剧的,但其在 COI 中的隔离及其与硬膜下腔脑脊液的连续性允许硬膜下输注抗炎治疗药物以抑制吞噬巨噬细胞浸润,从而提供神经保护。星形胶质细胞增生在遏制并最终消除创伤后严重破坏性炎症方面的作用似乎很明显,但尚未充分了解其可用于治疗性神经保护和神经再生策略。反应性星形胶质细胞的明显抗炎活性与其在清除因炎症而受损的血脑屏障中多余水肿液的积极作用相平行。最近阐明的神经创伤,包括 SCI、创伤性脑损伤 (TBI) 和中风的发病机制,要求在其治疗中采取以下主要治疗步骤以恢复神经功能:(1) 抑制和消除 COI 的破坏性炎症,伴随着血管源性水肿的减轻,(2) 在 COI 中插入支持再生轴突交叉的功能桥,(3) 通过暂时安全地去除白质目标区域的髓磷脂,使轴突再生到其原始突触目标,( 4) 体内连续治疗步骤的系统监测。本文的重点是治疗步骤 1。


























 京公网安备 11010802027423号
京公网安备 11010802027423号