Journal of Advanced Research ( IF 10.7 ) Pub Date : 2021-02-09 , DOI: 10.1016/j.jare.2021.01.018 Bufu Tang 1, 2 , Jinyu Zhu 1, 2 , Zhongwei Zhao 1, 3 , Chenying Lu 1, 3 , Siyu Liu 4 , Shiji Fang 3 , Liyun Zheng 3 , Nannan Zhang 1, 2 , Minjiang Chen 1, 3 , Min Xu 1, 3 , Risheng Yu 2 , Jiansong Ji 1, 3
|
Introduction
The development and prognosis of HCC involve complex molecular mechanisms, which affect the effectiveness of its treatment strategies. Tumor mutational burden (TMB) is related to the efficacy of immunotherapy, but the prognostic role of TMB-related genes in HCC has not yet been determined clearly.
Objectives
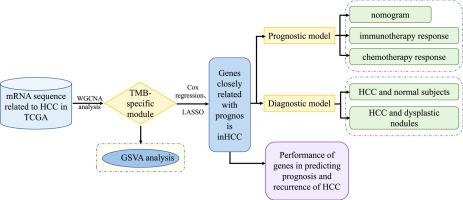
In this study, we identified TMB-specific genes with good prognostic value to build diagnostic and prognostic models and provide guidance for the treatment of HCC patients.
Methods
Weighted gene co-expression network analysis (WGCNA) was applied to identify the TMB-specific genes. And LASSO method and Cox regression were used in establishing the prognostic model.
Results
The prognostic model based on SMG5 and MRPL9 showed patients with higher prognostic risk had a remarkedly poorer survival probability than their counterparts with lower prognostic risk in both a TCGA cohort (P < 0.001, HR = 1.93) and an ICGC cohort (P < 0.001, HR = 3.58). In addition, higher infiltrating fractions of memory B cells, M0 macrophages, neutrophils, activated memory CD4 + T cells, follicular helper T cells and regulatory T cells and higher expression of B7H3, CTLA4, PD1, and TIM3 were present in the high-risk group than in the low-risk group (P < 0.05). Patients with high prognostic risk had higher resistance to some chemotherapy and targeted drugs, such as methotrexate, vinblastine and erlotinib, than those with low prognostic risk (P < 0.05). And a diagnostic model considering two genes was able to accurately distinguish patients with HCC from normal samples and those with dysplastic nodules. In addition, knockdown of SMG5 and MRPL9 was determined to significantly inhibit cell proliferation and migration in HCC.
Conclusion
Our study helps to select patients suitable for chemotherapy, targeted drugs and immunotherapy and provide new ideas for developing treatment strategies to improve disease outcomes in HCC patients.
中文翻译:

基于肿瘤突变负荷的肝细胞癌患者管理诊断和预后模型
介绍
HCC的发展和预后涉及复杂的分子机制,影响其治疗策略的有效性。肿瘤突变负荷(TMB)与免疫治疗的疗效有关,但 TMB 相关基因在 HCC 中的预后作用尚未明确。
目标
在这项研究中,我们确定了具有良好预后价值的 TMB 特异性基因,以建立诊断和预后模型,并为 HCC 患者的治疗提供指导。
方法
应用加权基因共表达网络分析 (WGCNA) 来鉴定 TMB 特异性基因。并采用LASSO方法和Cox回归建立预后模型。
结果
基于 SMG5 和 MRPL9 的预后模型显示,在 TCGA 队列(P < 0.001,HR = 1.93)和 ICGC 队列(P < 0.001,人力资源 = 3.58)。此外,在高危人群中,记忆 B 细胞、M0 巨噬细胞、中性粒细胞、活化记忆 CD4 + T 细胞、滤泡辅助 T 细胞和调节性 T 细胞的浸润分数较高,B7H3、CTLA4、PD1 和 TIM3 的表达较高。组高于低危组(P < 0.05)。与预后风险低的患者相比,预后风险高的患者对某些化疗和靶向药物(如甲氨蝶呤、长春碱和厄洛替尼)的耐药性更高(P < 0.05)。考虑到两个基因的诊断模型能够准确地区分 HCC 患者与正常样本和发育异常结节患者。此外,确定 SMG5 和 MRPL9 的敲低可显着抑制 HCC 中的细胞增殖和迁移。
结论
我们的研究有助于选择适合化疗、靶向药物和免疫治疗的患者,并为制定治疗策略以改善 HCC 患者的疾病预后提供新思路。


























 京公网安备 11010802027423号
京公网安备 11010802027423号