当前位置:
X-MOL 学术
›
J. Am. Coll. Cardiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Diastolic Function and Clinical Outcomes After Transcatheter Aortic Valve Replacement
Journal of the American College of Cardiology ( IF 24.0 ) Pub Date : 2020-12-01 , DOI: 10.1016/j.jacc.2020.10.032 Geraldine Ong , Philippe Pibarot , Bjorn Redfors , Neil J. Weissman , Wael A. Jaber , Raj R. Makkar , Stamatios Lerakis , Deepika Gopal , Omar Khalique , Susheel K. Kodali , Vinod H. Thourani , Saif Anwaruddin , Thomas McAndrew , Yiran Zhang , Maria C. Alu , Pamela S. Douglas , Rebecca T. Hahn
Journal of the American College of Cardiology ( IF 24.0 ) Pub Date : 2020-12-01 , DOI: 10.1016/j.jacc.2020.10.032 Geraldine Ong , Philippe Pibarot , Bjorn Redfors , Neil J. Weissman , Wael A. Jaber , Raj R. Makkar , Stamatios Lerakis , Deepika Gopal , Omar Khalique , Susheel K. Kodali , Vinod H. Thourani , Saif Anwaruddin , Thomas McAndrew , Yiran Zhang , Maria C. Alu , Pamela S. Douglas , Rebecca T. Hahn
|
BACKGROUND
Few studies have evaluated if diastolic function could predict outcomes in patients with aortic stenosis. OBJECTIVES
The authors aimed to assess the association between diastolic dysfunction (DD) and outcomes in patients with aortic stenosis undergoing transcatheter aortic valve replacement (TAVR). METHODS
Baseline, 30-day, and 1- and 2-year transthoracic echocardiograms from the PARTNER (Placement of Aortic Transcatheter Valves) 2 SAPIEN 3 registry were analyzed by a consortium of core laboratories and divided into the American Society of Echocardiography DD groups. RESULTS
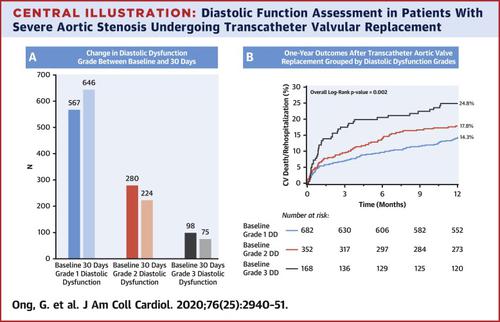
Among the 1,750 included, 682 (54.4%) had grade 1 DD, 352 (28.1%) had grade 2 DD, 168 (13.4%) had grade 3 DD, and 51 (4.1%) had indeterminate DD grade. Incremental baseline grades of DD were associated with an increase in combined 1- and 2-year cardiovascular (CV) death/rehospitalization (all p < 0.002) and all-cause death at 2 years (p = 0.01) but not at 1 year. Improvement in DD grade/grade 1 DD at 30 days post-TAVR was seen in 70.8% patients. Patients with improvement in ≥1 grade of DD/grade 1 DD had reduced 1-year CV death/rehospitalization (p < 0.001) and increased 2-year survival (p = 0.01). Baseline grade 3 DD was a predictor of 1-year CV death/rehospitalization (hazard ratio: 2.73; 95% confidence interval: 1.07 to 6.98; p = 0.04). Improvement in DD grade/grade 1 DD at 30 days was protective for 1-year CV death/rehospitalizations (hazard ratio: 0.39; 95% confidence interval: 0.19 to 0.83; p = 0.01). CONCLUSIONS
In the PARTNER 2 SAPIEN 3 registry, baseline DD was a predictor of up to 2 years clinical outcomes in patients who underwent TAVR. Improvement in DD grade at 30 days was associated with improvement in short-term clinical outcomes. (The PARTNER II Trial: Placement of AoRTic TraNscathetER Valves II - PARTNER II - PARTNERII - S3 Intermediate [PARTNERII S3i]; NCT03222128; PARTNER II Trial: Placement of AoRTic TraNscathetER Valves II - High Risk and Nested Registry 7 [PII S3HR/NR7]; NCT03222141).
中文翻译:

经导管主动脉瓣置换术后舒张功能和临床结果
背景 很少有研究评估舒张功能是否可以预测主动脉瓣狭窄患者的预后。目的 作者旨在评估舒张功能障碍 (DD) 与接受经导管主动脉瓣置换术 (TAVR) 的主动脉瓣狭窄患者结局之间的关联。方法 来自 PARTNER(主动脉经导管瓣膜放置)2 SAPIEN 3 登记处的基线、30 天和 1 年和 2 年经胸超声心动图由核心实验室联盟进行分析,并分为美国超声心动图学会 DD 组。结果 纳入的1750人中,682人(54.4%)为1级DD,352人(28.1%)为2级DD,168人(13.4%)为3级DD,51人(4.1%)为不确定DD级。DD 基线等级的增加与 1 年和 2 年心血管(CV)死亡/再住院(所有 p < 0.002)和 2 年全因死亡(p = 0.01)的增加有关,但与 1 年无关。70.8% 的患者在 TAVR 后 30 天观察到 DD 级/1 级 DD 的改善。≥ 1 级 DD/1 级 DD 改善的患者 1 年 CV 死亡/再入院率降低 (p < 0.001) 并增加 2 年生存率 (p = 0.01)。基线 3 级 DD 是 1 年 CV 死亡/再入院的预测因子(风险比:2.73;95% 置信区间:1.07 至 6.98;p = 0.04)。30 天 DD 等级/1 级 DD 的改善对 1 年 CV 死亡/再入院有保护作用(风险比:0.39;95% 置信区间:0.19 至 0.83;p = 0.01)。结论 在 PARTNER 2 SAPIEN 3 注册表中,在接受 TAVR 的患者中,基线 DD 是长达 2 年临床结果的预测因子。30 天 DD 等级的改善与短期临床结果的改善相关。(PARTNER II 试验:放置 AoRTic TraNscathetER 瓣膜 II - PARTNER II - PARTNERII - S3 Intermediate [PARTNERII S3i];NCT03222128;PARTNER II 试验:放置 AoRTic TraNscathetER 瓣膜 II - 高风险和嵌套注册 S3HR7 [NRPII] ; NCT03222141)。AoRTic TraNscathetER 瓣膜的放置 II - 高风险和嵌套注册 7 [PII S3HR/NR7];NCT03222141)。AoRTic TraNscathetER 瓣膜的放置 II - 高风险和嵌套注册 7 [PII S3HR/NR7];NCT03222141)。
更新日期:2020-12-01
中文翻译:

经导管主动脉瓣置换术后舒张功能和临床结果
背景 很少有研究评估舒张功能是否可以预测主动脉瓣狭窄患者的预后。目的 作者旨在评估舒张功能障碍 (DD) 与接受经导管主动脉瓣置换术 (TAVR) 的主动脉瓣狭窄患者结局之间的关联。方法 来自 PARTNER(主动脉经导管瓣膜放置)2 SAPIEN 3 登记处的基线、30 天和 1 年和 2 年经胸超声心动图由核心实验室联盟进行分析,并分为美国超声心动图学会 DD 组。结果 纳入的1750人中,682人(54.4%)为1级DD,352人(28.1%)为2级DD,168人(13.4%)为3级DD,51人(4.1%)为不确定DD级。DD 基线等级的增加与 1 年和 2 年心血管(CV)死亡/再住院(所有 p < 0.002)和 2 年全因死亡(p = 0.01)的增加有关,但与 1 年无关。70.8% 的患者在 TAVR 后 30 天观察到 DD 级/1 级 DD 的改善。≥ 1 级 DD/1 级 DD 改善的患者 1 年 CV 死亡/再入院率降低 (p < 0.001) 并增加 2 年生存率 (p = 0.01)。基线 3 级 DD 是 1 年 CV 死亡/再入院的预测因子(风险比:2.73;95% 置信区间:1.07 至 6.98;p = 0.04)。30 天 DD 等级/1 级 DD 的改善对 1 年 CV 死亡/再入院有保护作用(风险比:0.39;95% 置信区间:0.19 至 0.83;p = 0.01)。结论 在 PARTNER 2 SAPIEN 3 注册表中,在接受 TAVR 的患者中,基线 DD 是长达 2 年临床结果的预测因子。30 天 DD 等级的改善与短期临床结果的改善相关。(PARTNER II 试验:放置 AoRTic TraNscathetER 瓣膜 II - PARTNER II - PARTNERII - S3 Intermediate [PARTNERII S3i];NCT03222128;PARTNER II 试验:放置 AoRTic TraNscathetER 瓣膜 II - 高风险和嵌套注册 S3HR7 [NRPII] ; NCT03222141)。AoRTic TraNscathetER 瓣膜的放置 II - 高风险和嵌套注册 7 [PII S3HR/NR7];NCT03222141)。AoRTic TraNscathetER 瓣膜的放置 II - 高风险和嵌套注册 7 [PII S3HR/NR7];NCT03222141)。


























 京公网安备 11010802027423号
京公网安备 11010802027423号