当前位置:
X-MOL 学术
›
Clin. Exp. Immunol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Cervical cytomegalovirus reactivation, cytokines and spontaneous preterm birth in Kenyan women
Clinical & Experimental Immunology ( IF 4.6 ) Pub Date : 2020-12-03 , DOI: 10.1111/cei.13558 E R Begnel 1 , A L Drake 1, 2 , J Kinuthia 1, 3 , D Matemo 4 , M-L Huang 5 , K H Ásbjörnsdóttir 2 , V Chohan 6 , K Beima-Sofie 1 , G John-Stewart 1, 2, 6, 7 , D Lehman 1, 8 , J Slyker 1, 2
Clinical & Experimental Immunology ( IF 4.6 ) Pub Date : 2020-12-03 , DOI: 10.1111/cei.13558 E R Begnel 1 , A L Drake 1, 2 , J Kinuthia 1, 3 , D Matemo 4 , M-L Huang 5 , K H Ásbjörnsdóttir 2 , V Chohan 6 , K Beima-Sofie 1 , G John-Stewart 1, 2, 6, 7 , D Lehman 1, 8 , J Slyker 1, 2
Affiliation
|
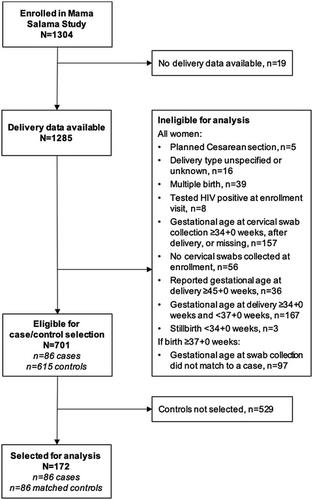
Genital cytomegalovirus (CMV) reactivation is common during the third trimester of pregnancy. We hypothesized that cervical CMV shedding may increase risk of spontaneous preterm birth (sPTB) through the release of inflammatory cytokines in the cervix. We conducted a nested case–control analysis to determine the relationship between CMV shedding and sPTB using data and samples from a prospective cohort study in western Kenya. Women who delivered between 28 + 0 and 33 + 6 weeks gestation were matched by gestational age at sample collection to controls who delivered ≥ 37 + 0 weeks. Levels of CMV DNA and interleukin (IL)‐1 beta (β), IL‐6, IL‐8 and tumor necrosis factor (TNF)‐α were measured in cervical swabs. We used conditional logistic regression to assess relationships between CMV shedding, cervical cytokine levels and sPTB. Among 86 cases and 86 matched controls, cervical CMV levels were not significantly associated with sPTB [odds ratio (OR) = 1·23, 95% confidence interval (CI) = 0·59–2·56], but were significantly associated with higher levels of cervical IL‐6 (β = 0·15, 95% CI = 0·02–0·29) and TNF‐α (β = 0·14, 95% CI = 0·01–0·27). In univariate analysis, higher odds of sPTB was associated with higher cervical IL‐6 levels (OR = 1·54, 95% CI = 1·00–2·38), but not with other cervical cytokines. In this cohort of Kenyan women, we did not find a significant association between cervical CMV shedding and sPTB before 34 weeks.
中文翻译:

肯尼亚妇女宫颈巨细胞病毒再激活、细胞因子和自发性早产
生殖器巨细胞病毒(CMV)重新激活在妊娠晚期很常见。我们假设宫颈巨细胞病毒脱落可能通过宫颈中炎症细胞因子的释放而增加自发性早产(sPTB)的风险。我们使用肯尼亚西部一项前瞻性队列研究的数据和样本进行了巢式病例对照分析,以确定 CMV 脱落与 sPTB 之间的关系。将孕期在 28 + 0 至 33 + 6 周之间分娩的女性按照样本采集时的孕龄与分娩≥ 37 + 0 周的对照进行匹配。测量宫颈拭子中 CMV DNA 和白细胞介素 (IL)-1 β (β)、IL-6、IL-8 和肿瘤坏死因子 (TNF)-α 的水平。我们使用条件逻辑回归来评估 CMV 脱落、宫颈细胞因子水平和 sPTB 之间的关系。在 86 例病例和 86 名匹配对照中,宫颈 CMV 水平与 sPTB 不显着相关[比值比 (OR) = 1·23,95% 置信区间 (CI) = 0·59–2·56],但与宫颈IL-6(β = 0·15,95% CI = 0·02–0·29)和TNF-α(β = 0·14,95% CI = 0·01–0·27)水平较高。在单变量分析中,较高的 sPTB 几率与较高的宫颈 IL-6 水平相关(OR = 1·54,95% CI = 1·00–2·38),但与其他宫颈细胞因子无关。在这组肯尼亚女性中,我们没有发现 34 周之前宫颈 CMV 脱落与 sPTB 之间存在显着关联。
更新日期:2021-02-10
中文翻译:

肯尼亚妇女宫颈巨细胞病毒再激活、细胞因子和自发性早产
生殖器巨细胞病毒(CMV)重新激活在妊娠晚期很常见。我们假设宫颈巨细胞病毒脱落可能通过宫颈中炎症细胞因子的释放而增加自发性早产(sPTB)的风险。我们使用肯尼亚西部一项前瞻性队列研究的数据和样本进行了巢式病例对照分析,以确定 CMV 脱落与 sPTB 之间的关系。将孕期在 28 + 0 至 33 + 6 周之间分娩的女性按照样本采集时的孕龄与分娩≥ 37 + 0 周的对照进行匹配。测量宫颈拭子中 CMV DNA 和白细胞介素 (IL)-1 β (β)、IL-6、IL-8 和肿瘤坏死因子 (TNF)-α 的水平。我们使用条件逻辑回归来评估 CMV 脱落、宫颈细胞因子水平和 sPTB 之间的关系。在 86 例病例和 86 名匹配对照中,宫颈 CMV 水平与 sPTB 不显着相关[比值比 (OR) = 1·23,95% 置信区间 (CI) = 0·59–2·56],但与宫颈IL-6(β = 0·15,95% CI = 0·02–0·29)和TNF-α(β = 0·14,95% CI = 0·01–0·27)水平较高。在单变量分析中,较高的 sPTB 几率与较高的宫颈 IL-6 水平相关(OR = 1·54,95% CI = 1·00–2·38),但与其他宫颈细胞因子无关。在这组肯尼亚女性中,我们没有发现 34 周之前宫颈 CMV 脱落与 sPTB 之间存在显着关联。

























 京公网安备 11010802027423号
京公网安备 11010802027423号