当前位置:
X-MOL 学术
›
NMR Biomed.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Liver perfusion MRI in a rodent model of cirrhosis: Agreement with bulk‐flow phase‐contrast MRI and noninvasive evaluation of inflammation in chronic liver disease using flow‐sensitive alternating inversion recovery arterial spin labelling and tissue T1
NMR in Biomedicine ( IF 2.9 ) Pub Date : 2020-10-07 , DOI: 10.1002/nbm.4423 Manil Dinesh Chouhan 1 , Rajiv Ramasawmy 1 , Alan Bainbridge 1 , Adrienne Campbell-Washburn 1 , Steve Halligan 1 , Nathan Davies 1 , Simon Walker-Samuel 1 , Mark F Lythgoe 1 , Rajeshwar Prosad Mookerjee 1 , Stuart Andrew Taylor 1
NMR in Biomedicine ( IF 2.9 ) Pub Date : 2020-10-07 , DOI: 10.1002/nbm.4423 Manil Dinesh Chouhan 1 , Rajiv Ramasawmy 1 , Alan Bainbridge 1 , Adrienne Campbell-Washburn 1 , Steve Halligan 1 , Nathan Davies 1 , Simon Walker-Samuel 1 , Mark F Lythgoe 1 , Rajeshwar Prosad Mookerjee 1 , Stuart Andrew Taylor 1
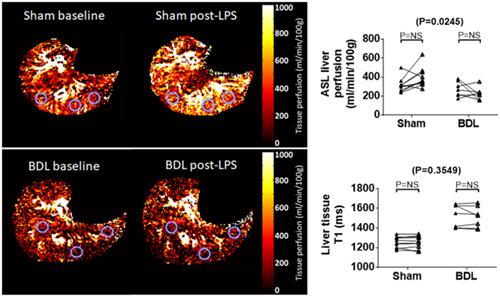
Affiliation
|
Noninvasive measurements of liver perfusion and fibrosis in cirrhotic small animals can help develop treatments for haemodynamic complications of liver disease. Here, we measure liver perfusion in cirrhotic rodents using flow‐sensitive alternating inversion recovery arterial spin labelling (FAIR ASL), evaluating agreement with previously validated caval subtraction phase‐contrast magnetic resonance imaging (PCMRI) total liver blood flow (TLBF). Baseline differences in cirrhotic rodents and the haemodynamic effects of acute inflammation were investigated using FAIR ASL and tissue T1. Sprague–Dawley rats (nine bile duct ligated [BDL] and ten sham surgery controls) underwent baseline hepatic FAIR ASL with T1 measurement and caval subtraction PCMRI (with two‐dimensional infra‐/supra‐hepatic inferior vena caval studies), induction of inflammation with intravenous lipopolysaccharide (LPS) and repeat liver FAIR ASL with T1 measurement after ~90 minutes. The mean difference between FAIR ASL hepatic perfusion and caval subtraction PCMRI TLBF was −51 ± 30 ml/min/100 g (Bland–Altman 95% limits‐of‐agreement ±258 ml/min/100 g). The FAIR ASL coefficient of variation was smaller than for caval subtraction PCMRI (29.3% vs 50.1%; P = .03). At baseline, FAIR ASL liver perfusion was lower in BDL rats (199 ± 32 ml/min/100 g vs sham 316 ± 24 ml/min/100 g; P = .01) but liver T1 was higher (BDL 1533 ± 50 vs sham 1256 ± 18 ms; P = .0004). Post‐LPS FAIR ASL liver perfusion response differences were observed between sham/BDL rats (P = .02), approaching significance in sham (+78 ± 33 ml/min/100 g; P = .06) but not BDL rats (−49 ± 40 ml/min/100 g; P = .47). Post‐LPS differences in liver tissue T1 were nonsignificant (P = .35). FAIR ASL hepatic perfusion and caval subtraction PCMRI TLBF agreement was modest, with significant baseline FAIR ASL liver perfusion and tissue T1 differences in rodents with advanced cirrhosis compared with controls. Following inflammatory stress, differences in hepatic perfusion response were detected between cirrhotic/control animals, but liver T1 was unaffected. Findings underline the potential of FAIR ASL in the assessment of vasoactive treatments for patients with chronic liver disease and inflammation.
中文翻译:

肝硬化啮齿动物模型中的肝灌注 MRI:与大流量相位对比 MRI 一致,并使用流量敏感交替反转恢复动脉自旋标记和组织 T1 对慢性肝病炎症进行无创评估
对肝硬化小动物的肝灌注和纤维化进行无创测量可以帮助开发治疗肝病血流动力学并发症的方法。在这里,我们使用流动敏感交替反转恢复动脉自旋标记 (FAIR ASL) 测量肝硬化啮齿动物的肝脏灌注,评估与先前验证的腔静脉减影相衬磁共振成像 (PCMRI) 总肝血流量 (TLBF) 的一致性。使用 FAIR ASL 和组织 T1 研究肝硬化啮齿动物的基线差异和急性炎症的血流动力学影响。Sprague-Dawley 大鼠(9 只胆管结扎 [BDL] 和 10 只假手术对照组)接受基线肝脏 FAIR ASL,T1 测量和腔静脉减影 PCMRI(二维下/肝上下腔静脉研究),用静脉内脂多糖 (LPS) 诱导炎症,并在约 90 分钟后重复肝脏 FAIR ASL 和 T1 测量。FAIR ASL 肝灌注和腔静脉减影 PCMRI TLBF 之间的平均差异为 -51 ± 30 ml/min/100 g(Bland-Altman 95% 协议限制 ±258 ml/min/100 g)。FAIR ASL 变异系数小于腔静脉减影 PCMRI(29.3% vs 50.1%;P = .03)。在基线时,BDL 大鼠的 FAIR ASL 肝脏灌注较低(199 ± 32 ml/min/100 g vs 假手术 316 ± 24 ml/min/100 g;P = .01)但肝脏 T1 较高(BDL 1533 ± 50 vs假 1256 ± 18 毫秒;P = .0004)。在假手术/BDL 大鼠之间观察到 LPS FAIR ASL 肝灌注反应差异 ( P = .02),在假手术 (+78 ± 33 ml/min/100 g; P = .06) 中接近显着性,但在 BDL 大鼠中没有差异 (- 49 ± 40 毫升/分钟/100 克;P = .47)。LPS 后肝组织 T1 的差异不显着(P= .35)。FAIR ASL 肝灌注和腔静脉减影 PCMRI TLBF 一致性适中,与对照组相比,晚期肝硬化啮齿动物的 FAIR ASL 肝灌注和组织 T1 差异显着。炎症应激后,在肝硬化/对照动物之间检测到肝脏灌注反应的差异,但肝脏 T1 不受影响。研究结果强调了 FAIR ASL 在评估慢性肝病和炎症患者血管活性治疗方面的潜力。
更新日期:2020-10-07
中文翻译:

肝硬化啮齿动物模型中的肝灌注 MRI:与大流量相位对比 MRI 一致,并使用流量敏感交替反转恢复动脉自旋标记和组织 T1 对慢性肝病炎症进行无创评估
对肝硬化小动物的肝灌注和纤维化进行无创测量可以帮助开发治疗肝病血流动力学并发症的方法。在这里,我们使用流动敏感交替反转恢复动脉自旋标记 (FAIR ASL) 测量肝硬化啮齿动物的肝脏灌注,评估与先前验证的腔静脉减影相衬磁共振成像 (PCMRI) 总肝血流量 (TLBF) 的一致性。使用 FAIR ASL 和组织 T1 研究肝硬化啮齿动物的基线差异和急性炎症的血流动力学影响。Sprague-Dawley 大鼠(9 只胆管结扎 [BDL] 和 10 只假手术对照组)接受基线肝脏 FAIR ASL,T1 测量和腔静脉减影 PCMRI(二维下/肝上下腔静脉研究),用静脉内脂多糖 (LPS) 诱导炎症,并在约 90 分钟后重复肝脏 FAIR ASL 和 T1 测量。FAIR ASL 肝灌注和腔静脉减影 PCMRI TLBF 之间的平均差异为 -51 ± 30 ml/min/100 g(Bland-Altman 95% 协议限制 ±258 ml/min/100 g)。FAIR ASL 变异系数小于腔静脉减影 PCMRI(29.3% vs 50.1%;P = .03)。在基线时,BDL 大鼠的 FAIR ASL 肝脏灌注较低(199 ± 32 ml/min/100 g vs 假手术 316 ± 24 ml/min/100 g;P = .01)但肝脏 T1 较高(BDL 1533 ± 50 vs假 1256 ± 18 毫秒;P = .0004)。在假手术/BDL 大鼠之间观察到 LPS FAIR ASL 肝灌注反应差异 ( P = .02),在假手术 (+78 ± 33 ml/min/100 g; P = .06) 中接近显着性,但在 BDL 大鼠中没有差异 (- 49 ± 40 毫升/分钟/100 克;P = .47)。LPS 后肝组织 T1 的差异不显着(P= .35)。FAIR ASL 肝灌注和腔静脉减影 PCMRI TLBF 一致性适中,与对照组相比,晚期肝硬化啮齿动物的 FAIR ASL 肝灌注和组织 T1 差异显着。炎症应激后,在肝硬化/对照动物之间检测到肝脏灌注反应的差异,但肝脏 T1 不受影响。研究结果强调了 FAIR ASL 在评估慢性肝病和炎症患者血管活性治疗方面的潜力。



























 京公网安备 11010802027423号
京公网安备 11010802027423号