当前位置:
X-MOL 学术
›
J. Am. Coll. Cardiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
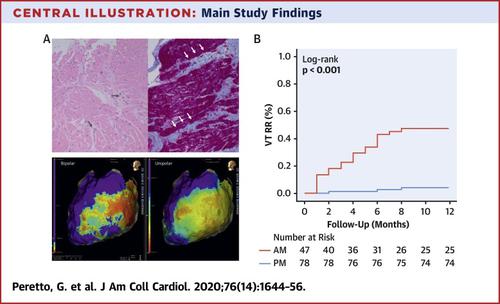
Inflammation as a Predictor of Recurrent Ventricular Tachycardia After Ablation in Patients With Myocarditis
Journal of the American College of Cardiology ( IF 24.0 ) Pub Date : 2020-10-01 , DOI: 10.1016/j.jacc.2020.08.012 Giovanni Peretto , Simone Sala , Cristina Basso , Stefania Rizzo , Andrea Radinovic , Antonio Frontera , Luca Rosario Limite , Gabriele Paglino , Caterina Bisceglia , Giacomo De Luca , Corrado Campochiaro , Silvia Sartorelli , Anna Palmisano , Antonio Esposito , Elena Busnardo , Andrea Villatore , Francesca Baratto , Manuela Cireddu , Alessandra Marzi , Giuseppe D’Angelo , Simone Gulletta , Pasquale Vergara , Francesco De Cobelli , Lorenzo Dagna , Patrizio Mazzone , Paolo Della Bella
Journal of the American College of Cardiology ( IF 24.0 ) Pub Date : 2020-10-01 , DOI: 10.1016/j.jacc.2020.08.012 Giovanni Peretto , Simone Sala , Cristina Basso , Stefania Rizzo , Andrea Radinovic , Antonio Frontera , Luca Rosario Limite , Gabriele Paglino , Caterina Bisceglia , Giacomo De Luca , Corrado Campochiaro , Silvia Sartorelli , Anna Palmisano , Antonio Esposito , Elena Busnardo , Andrea Villatore , Francesca Baratto , Manuela Cireddu , Alessandra Marzi , Giuseppe D’Angelo , Simone Gulletta , Pasquale Vergara , Francesco De Cobelli , Lorenzo Dagna , Patrizio Mazzone , Paolo Della Bella
|
BACKGROUND
Little is known about the risk stratification of patients with myocarditis undergoing ventricular tachycardia (VT) ablation. OBJECTIVES
This study sought to describe VT ablation results and identify factors associated with arrhythmia recurrences in a cohort of patients with myocarditis. METHODS
The authors enrolled 125 consecutive patients with myocarditis, undergoing VT ablation. Before ablation, disease stage was evaluated, to identify active (AM) versus previous myocarditis (PM). The primary study endpoint was assessment of VT recurrences by 12-month follow-up. Predictors of VT recurrences were retrospectively identified. RESULTS
All patients (age 51 ± 14 years, 91% men, left ventricular ejection fraction 52% ± 9%) had history of myocarditis diagnosed by endomyocardial biopsy (59%) and/or cardiac magnetic resonance (90%). Furthermore, all had multiple episodes of drug-refractory VTs. Multimodal pre-procedural staging identified 47 patients with AM (38%) and 78 patients with PM (62%). All patients showed low-voltage areas (LVA) at electroanatomical map (97% epicardial or endoepicardial); of them, 25 (20%) had wide borderzone (WBZ, constituting >50% of the whole LVA). VT recurrences were documented in 25 patients (20%) by 12 months, and in 43 (34%) by last follow-up (median 63 months; interquartile range: 39 to 87). At multivariable analysis, AM stage was the only predictor of VT recurrences by 12 months (hazard ratio: 9.5; 95% confidence interval: 2.6 to 35.3; p < 0.001), whereas both AM stage and WBZ were associated with arrhythmia recurrences anytime during follow-up. No VT episodes were found after redo ablation was performed in 23 patients during PM stage. CONCLUSION
Our findings suggest that VT ablation should be avoided during AM, but is often of benefit for recurrent VT after the acute phase of myocarditis.
中文翻译:

炎症是心肌炎患者消融后复发性室性心动过速的预测因素
背景 对于接受室性心动过速 (VT) 消融的心肌炎患者的风险分层知之甚少。目的 本研究旨在描述一组心肌炎患者的 VT 消融结果并确定与心律失常复发相关的因素。方法 作者连续招募了 125 名接受 VT 消融的心肌炎患者。在消融之前,评估疾病阶段,以确定活动性 (AM) 与既往心肌炎 (PM)。主要研究终点是通过 12 个月的随访评估 VT 复发。VT 复发的预测因子被回顾性地确定。结果 所有患者(年龄 51 ± 14 岁,91% 男性,左心室射血分数 52% ± 9%)都有通过心内膜心肌活检 (59%) 和/或心脏磁共振 (90%) 诊断出的心肌炎病史。此外,所有人都有多次药物难治性 VT 发作。多模式术前分期确定了 47 名 AM 患者 (38%) 和 78 名 PM 患者 (62%)。所有患者在电解剖图上均显示低电压区(LVA)(97%为心外膜或心内膜);其中,25 个(20%)具有宽边界带(WBZ,占整个 LVA 的 50% 以上)。到 12 个月时,记录了 25 名患者 (20%) 和 43 名 (34%) 到最后一次随访(中位数 63 个月;四分位距:39 至 87)的 VT 复发。在多变量分析中,AM 分期是 12 个月内 VT 复发的唯一预测因素(风险比:9.5;95% 置信区间:2.6 至 35.3;p < 0.001),而 AM 分期和 WBZ 均与随访期间任何时间的心律失常复发相关-向上。23 名患者在 PM 阶段进行重做消融后未发现 VT 发作。
更新日期:2020-10-01
中文翻译:

炎症是心肌炎患者消融后复发性室性心动过速的预测因素
背景 对于接受室性心动过速 (VT) 消融的心肌炎患者的风险分层知之甚少。目的 本研究旨在描述一组心肌炎患者的 VT 消融结果并确定与心律失常复发相关的因素。方法 作者连续招募了 125 名接受 VT 消融的心肌炎患者。在消融之前,评估疾病阶段,以确定活动性 (AM) 与既往心肌炎 (PM)。主要研究终点是通过 12 个月的随访评估 VT 复发。VT 复发的预测因子被回顾性地确定。结果 所有患者(年龄 51 ± 14 岁,91% 男性,左心室射血分数 52% ± 9%)都有通过心内膜心肌活检 (59%) 和/或心脏磁共振 (90%) 诊断出的心肌炎病史。此外,所有人都有多次药物难治性 VT 发作。多模式术前分期确定了 47 名 AM 患者 (38%) 和 78 名 PM 患者 (62%)。所有患者在电解剖图上均显示低电压区(LVA)(97%为心外膜或心内膜);其中,25 个(20%)具有宽边界带(WBZ,占整个 LVA 的 50% 以上)。到 12 个月时,记录了 25 名患者 (20%) 和 43 名 (34%) 到最后一次随访(中位数 63 个月;四分位距:39 至 87)的 VT 复发。在多变量分析中,AM 分期是 12 个月内 VT 复发的唯一预测因素(风险比:9.5;95% 置信区间:2.6 至 35.3;p < 0.001),而 AM 分期和 WBZ 均与随访期间任何时间的心律失常复发相关-向上。23 名患者在 PM 阶段进行重做消融后未发现 VT 发作。


























 京公网安备 11010802027423号
京公网安备 11010802027423号