JACC: Heart Failure ( IF 13.0 ) Pub Date : 2020-09-09 , DOI: 10.1016/j.jchf.2020.06.015 Luis E Rohde 1 , Neal A Chatterjee 2 , Muthiah Vaduganathan 3 , Brian Claggett 3 , Milton Packer 4 , Akshay S Desai 3 , Michael Zile 5 , Jean Rouleau 6 , Karl Swedberg 7 , Martin Lefkowitz 8 , Victor Shi 8 , John J V McMurray 9 , Scott D Solomon 3
|
Objectives
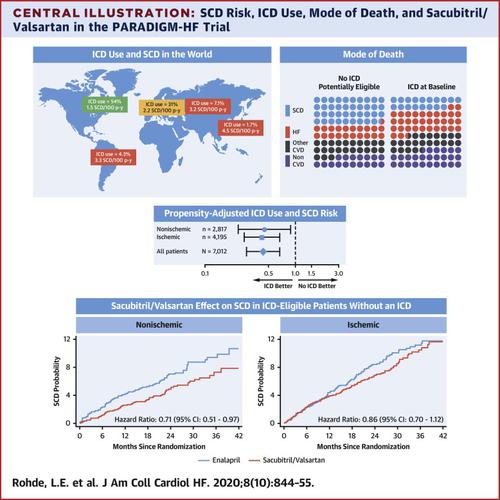
The purpose of this study was to investigate the effect of sacubitril/valsartan therapy on sudden cardiac death (SCD) according to the use of and eligibility for an implantable cardioverter-defibrillator (ICD), stratified by heart failure cause.
Background
SCD still accounts for a significant proportion of overall mortality in heart failure with reduced ejection fraction (HFrEF).
Methods
Patients enrolled in the PARADIGM-HF (Prospective Comparison of ARNI with an ACE-Inhibitor to Determine Impact on Global Mortality and Morbidity in Heart Failure) trial (n = 8,399) were evaluated to assess patterns of ICD implantation and eligibility according to clinical guidelines. The impact of ICD (adjusted for propensity of ICD implantation) and sacubitril/valsartan therapy on SCD was evaluated by using cause-specific Cox models and competing risk analysis.
Results
At baseline, of the 7,145 patients (85%) eligible for ICD implantation, only 1,243 (15%) had an ICD. Use of ICD varied by region with the highest rates in North America (56%) and lowest in Asia-Pacific (1.7%). In a propensity score-adjusted analysis, use of an ICD was associated with a 56% lower risk of SCD in ICD-eligible patients, in both patients with ischemic (p < 0.001) and nonischemic cardiomyopathy (p = 0.02). Sacubitril/valsartan reduced SCD risk in patients with an ICD (hazard ratio [HR]: 0.49; 95% confidence interval [CI]: 0.25 to 0.99) and in those who were eligible for but did not receive an ICD (HR: 0.81; 95% CI: 0.67 to 0.98). This effect was particularly evident in nonischemic cardiomyopathy (p < 0.05), although interaction with the cause of HF was not significant (p = 0.11 in subjects using an ICD and p = 0.25 in eligible nonusers).
Conclusions
Use of an ICD was associated with lower rates of SCD, regardless of HF cause but was underused in most regions of the world in the PARADIGM-HF study. Sacubitril/valsartan reduced SCD risk regardless of use of an ICD or eligibility, particularly in ICD users and nonischemic cardiomyopathy.
中文翻译:

沙库巴曲/缬沙坦和根据植入式心脏复律除颤器使用和心力衰竭的心脏猝死原因:PARADIGM-HF 分析。
目标
本研究的目的是根据植入式心脏复律除颤器 (ICD) 的使用和资格,根据心力衰竭原因进行分层,研究沙库巴曲/缬沙坦治疗对心源性猝死 (SCD) 的影响。
背景
SCD 仍占射血分数降低的心力衰竭 (HFrEF) 总死亡率的很大一部分。
方法
根据临床指南,对参加 PARADIGM-HF(ARNI 与 ACE 抑制剂对确定对全球死亡率和心力衰竭发病率的影响的前瞻性比较)试验(n = 8,399)的患者进行评估,以评估 ICD 植入的模式和资格。通过使用病因特异性 Cox 模型和竞争风险分析评估 ICD(根据 ICD 植入倾向调整)和沙库巴曲/缬沙坦治疗对 SCD 的影响。
结果
在基线时,在符合 ICD 植入条件的 7,145 名患者 (85%) 中,只有 1,243 (15%) 名患者有 ICD。ICD 的使用因地区而异,北美最高 (56%),亚太地区最低 (1.7%)。在倾向评分调整后的分析中,无论是缺血性心肌病(p < 0.001)还是非缺血性心肌病(p = 0.02),ICD 合格患者的 SCD 风险均降低了 56%。沙库巴曲/缬沙坦降低了 ICD 患者的 SCD 风险(风险比 [HR]:0.49;95% 置信区间 [CI]:0.25 至 0.99)和符合条件但未接受 ICD 的患者(HR:0.81; 95% 置信区间:0.67 至 0.98)。这种影响在非缺血性心肌病中尤为明显(p < 0.05),尽管与 HF 的相互作用不显着(在使用 ICD 的受试者中 p = 0.11 和 p = 0。
结论
无论心衰原因如何,ICD 的使用与 SCD 的发生率较低有关,但在 PARADIGM-HF 研究中,在世界大部分地区未得到充分利用。无论是否使用 ICD 或是否合格,沙库巴曲/缬沙坦都降低了 SCD 风险,特别是在 ICD 使用者和非缺血性心肌病中。

























 京公网安备 11010802027423号
京公网安备 11010802027423号