当前位置:
X-MOL 学术
›
Ann. N. Y. Acad. Sci.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Targeting the β‐adrenergic receptor in the clinical management of congenital long QT syndrome
Annals of the New York Academy of Sciences ( IF 5.2 ) Pub Date : 2020-07-07 , DOI: 10.1111/nyas.14425 Khalil Saadeh 1, 2 , Kalyanam Shivkumar 3 , Kamalan Jeevaratnam 1
Annals of the New York Academy of Sciences ( IF 5.2 ) Pub Date : 2020-07-07 , DOI: 10.1111/nyas.14425 Khalil Saadeh 1, 2 , Kalyanam Shivkumar 3 , Kamalan Jeevaratnam 1
Affiliation
|
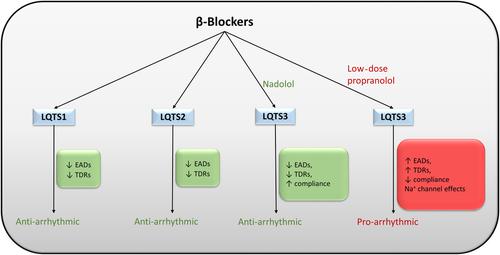
The long QT syndrome (LQTS) is largely treated pharmacologically with β-blockers, despite the role of sympathetic activity in LQTS being poorly understood. Using the trigger-substrate model of cardiac arrhythmias in this review, we amalgamate current experimental and clinical data from both animal and human studies to explain the mechanism of adrenergic stimulation and blockade on LQT arrhythmic risk and hence assess the efficacy of β-adrenoceptor blockade in the management of LQTS. In LQTS1 and LQTS2, sympathetic stimulation increases arrhythmic risk by enhancing early afterdepolarizations and transmural dispersion of repolarization. β-Blockers successfully reduce cardiac events by reducing these triggers and substrates; however, these effects are less marked in LQTS2 compared with LQTS1. In LQTS3, clinical and experimental investigations of the effects of sympathetic stimulation and β-blocker use have produced contradictory findings, resulting in significant clinical uncertainty. We offer explanations for these contradicting results relating to study sample size, the dose of the β-blocker administered associated with its off-target Na+ channel effects, as well as the type of β-blocker used. We conclude that the antiarrhythmic efficacy of β-blockers is a genotype-specific phenomenon, and hence the use of β-blockers in clinical practice should be genotype dependent.
中文翻译:

在先天性长 QT 综合征临床治疗中靶向 β-肾上腺素能受体
尽管交感神经活动在 LQTS 中的作用知之甚少,但长 QT 综合征 (LQTS) 主要用 β 受体阻滞剂进行药物治疗。在本综述中使用心律失常的触发底物模型,我们合并了来自动物和人类研究的当前实验和临床数据,以解释肾上腺素能刺激和阻断对 LQT 心律失常风险的机制,从而评估β-肾上腺素能受体阻断剂在LQTS 的管理。在 LQTS1 和 LQTS2 中,交感神经刺激通过增强早期后去极化和再极化的透壁分散来增加心律失常的风险。β-受体阻滞剂通过减少这些触发因素和底物成功减少心脏事件;然而,与 LQTS1 相比,这些影响在 LQTS2 中不那么明显。在 LQTS3 中,对交感神经刺激和 β 受体阻滞剂使用影响的临床和实验研究产生了相互矛盾的结果,导致显着的临床不确定性。我们对这些相互矛盾的结果提供了解释,这些结果与研究样本量、与脱靶 Na+ 通道效应相关的 β-受体阻滞剂的给药剂量以及所用β-受体阻滞剂的类型有关。我们得出结论,β-受体阻滞剂的抗心律失常功效是一种基因型特异性现象,因此临床实践中β-受体阻滞剂的使用应具有基因型依赖性。β-受体阻滞剂的给药剂量与其脱靶 Na+ 通道效应相关,以及所用β-受体阻滞剂的类型。我们得出结论,β-受体阻滞剂的抗心律失常功效是一种基因型特异性现象,因此临床实践中β-受体阻滞剂的使用应具有基因型依赖性。β-受体阻滞剂的给药剂量与其脱靶 Na+ 通道效应相关,以及所用β-受体阻滞剂的类型。我们得出结论,β-受体阻滞剂的抗心律失常功效是一种基因型特异性现象,因此临床实践中β-受体阻滞剂的使用应具有基因型依赖性。
更新日期:2020-07-07
中文翻译:

在先天性长 QT 综合征临床治疗中靶向 β-肾上腺素能受体
尽管交感神经活动在 LQTS 中的作用知之甚少,但长 QT 综合征 (LQTS) 主要用 β 受体阻滞剂进行药物治疗。在本综述中使用心律失常的触发底物模型,我们合并了来自动物和人类研究的当前实验和临床数据,以解释肾上腺素能刺激和阻断对 LQT 心律失常风险的机制,从而评估β-肾上腺素能受体阻断剂在LQTS 的管理。在 LQTS1 和 LQTS2 中,交感神经刺激通过增强早期后去极化和再极化的透壁分散来增加心律失常的风险。β-受体阻滞剂通过减少这些触发因素和底物成功减少心脏事件;然而,与 LQTS1 相比,这些影响在 LQTS2 中不那么明显。在 LQTS3 中,对交感神经刺激和 β 受体阻滞剂使用影响的临床和实验研究产生了相互矛盾的结果,导致显着的临床不确定性。我们对这些相互矛盾的结果提供了解释,这些结果与研究样本量、与脱靶 Na+ 通道效应相关的 β-受体阻滞剂的给药剂量以及所用β-受体阻滞剂的类型有关。我们得出结论,β-受体阻滞剂的抗心律失常功效是一种基因型特异性现象,因此临床实践中β-受体阻滞剂的使用应具有基因型依赖性。β-受体阻滞剂的给药剂量与其脱靶 Na+ 通道效应相关,以及所用β-受体阻滞剂的类型。我们得出结论,β-受体阻滞剂的抗心律失常功效是一种基因型特异性现象,因此临床实践中β-受体阻滞剂的使用应具有基因型依赖性。β-受体阻滞剂的给药剂量与其脱靶 Na+ 通道效应相关,以及所用β-受体阻滞剂的类型。我们得出结论,β-受体阻滞剂的抗心律失常功效是一种基因型特异性现象,因此临床实践中β-受体阻滞剂的使用应具有基因型依赖性。



























 京公网安备 11010802027423号
京公网安备 11010802027423号