当前位置:
X-MOL 学术
›
Ann. N. Y. Acad. Sci.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
How to approach esophagogastric junction outflow obstruction?
Annals of the New York Academy of Sciences ( IF 5.2 ) Pub Date : 2020-06-17 , DOI: 10.1111/nyas.14412 Tanisa Patcharatrakul 1, 2 , Ahmad Alkaddour 3 , Panyavee Pitisuttithum 4 , Sureeporn Jangsirikul 2 , Kenneth J Vega 3 , John O Clarke 5 , Sutep Gonlachanvit 1, 2
Annals of the New York Academy of Sciences ( IF 5.2 ) Pub Date : 2020-06-17 , DOI: 10.1111/nyas.14412 Tanisa Patcharatrakul 1, 2 , Ahmad Alkaddour 3 , Panyavee Pitisuttithum 4 , Sureeporn Jangsirikul 2 , Kenneth J Vega 3 , John O Clarke 5 , Sutep Gonlachanvit 1, 2
Affiliation
|
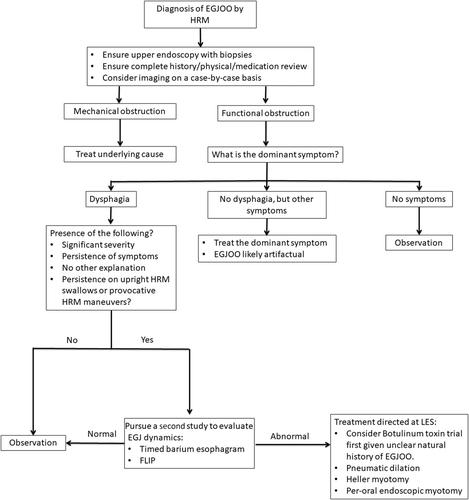
The diagnosis of esophagogastric junction outflow obstruction (EGJOO) is currently based on high‐resolution esophageal manometry and is characterized by impaired EGJ relaxation with preserved esophageal peristalsis. This condition has been defined by the Chicago Classification as a major esophageal motility disorder, although its clinical significance is controversial since heterogeneous and irrelevant presentations have been reported. EGJOO commonly has a benign clinical course, with spontaneous resolution, but it can also be associated with opioid usage, early achalasia, and mechanical obstruction. A careful medical, surgical, and medication history coupled with a careful manometry interpretation focused on the factors that might affect the integrated relaxation pressure are the keys for an accurate diagnosis. The advance of esophageal physiological tests can evaluate the clearance of the esophageal contents across the EGJ. The manometry technique, including testing in an upright position and provocative tests, can also complement those tests and demonstrate the evidence of EGJ obstruction. After making a diagnosis, endoscopy should be an initial step to exclude anatomical causes if it has not yet been done. Imaging studies can identify infiltrative lesions, but the reported diagnostic yield is relatively low. Management of EGJOO depends on the underlying etiology. Functional EGJOO patients with persistent dysphagia associated with the presence of outflow obstruction may require EGJ disruption therapy.
中文翻译:

如何处理食管胃交界处流出道梗阻?
食管胃交界处流出道梗阻(EGJOO)的诊断目前基于高分辨率食管测压法,其特征是 EGJ 松弛受损,食管蠕动保留。这种情况已被芝加哥分类定义为主要的食管动力障碍,尽管由于报告了异质性和不相关的表现,因此其临床意义存在争议。EGJOO 通常具有良性临床病程,可自发消退,但也可能与阿片类药物使用、早期贲门失弛缓症和机械性梗阻有关。仔细的医疗、手术和用药史,再加上对可能影响综合松弛压力的因素的仔细测压解释,是准确诊断的关键。食管生理学检查的进展可以评估食管内容物在 EGJ 的清除情况。测压技术,包括直立位置测试和刺激测试,也可以补充这些测试并证明 EGJ 阻塞的证据。做出诊断后,内窥镜检查应该是排除解剖学原因(如果尚未进行)的第一步。影像学研究可以识别浸润性病变,但报告的诊断率相对较低。EGJOO 的管理取决于潜在的病因。伴有流出道梗阻的持续吞咽困难的功能性 EGJOO 患者可能需要 EGJ 中断治疗。包括直立位置测试和刺激测试,也可以补充这些测试并证明 EGJ 阻塞的证据。做出诊断后,内窥镜检查应该是排除解剖学原因(如果尚未进行)的第一步。影像学研究可以识别浸润性病变,但报告的诊断率相对较低。EGJOO 的管理取决于潜在的病因。伴有流出道梗阻的持续吞咽困难的功能性 EGJOO 患者可能需要 EGJ 中断治疗。包括直立位测试和刺激测试,也可以补充这些测试并证明 EGJ 阻塞的证据。做出诊断后,内窥镜检查应该是排除解剖学原因(如果尚未进行)的第一步。影像学研究可以识别浸润性病变,但报告的诊断率相对较低。EGJOO 的管理取决于潜在的病因。伴有流出道梗阻的持续吞咽困难的功能性 EGJOO 患者可能需要 EGJ 中断治疗。但报告的诊断率相对较低。EGJOO 的管理取决于潜在的病因。伴有流出道梗阻的持续吞咽困难的功能性 EGJOO 患者可能需要 EGJ 中断治疗。但报告的诊断率相对较低。EGJOO 的管理取决于潜在的病因。伴有流出道梗阻的持续吞咽困难的功能性 EGJOO 患者可能需要 EGJ 中断治疗。
更新日期:2020-06-17
中文翻译:

如何处理食管胃交界处流出道梗阻?
食管胃交界处流出道梗阻(EGJOO)的诊断目前基于高分辨率食管测压法,其特征是 EGJ 松弛受损,食管蠕动保留。这种情况已被芝加哥分类定义为主要的食管动力障碍,尽管由于报告了异质性和不相关的表现,因此其临床意义存在争议。EGJOO 通常具有良性临床病程,可自发消退,但也可能与阿片类药物使用、早期贲门失弛缓症和机械性梗阻有关。仔细的医疗、手术和用药史,再加上对可能影响综合松弛压力的因素的仔细测压解释,是准确诊断的关键。食管生理学检查的进展可以评估食管内容物在 EGJ 的清除情况。测压技术,包括直立位置测试和刺激测试,也可以补充这些测试并证明 EGJ 阻塞的证据。做出诊断后,内窥镜检查应该是排除解剖学原因(如果尚未进行)的第一步。影像学研究可以识别浸润性病变,但报告的诊断率相对较低。EGJOO 的管理取决于潜在的病因。伴有流出道梗阻的持续吞咽困难的功能性 EGJOO 患者可能需要 EGJ 中断治疗。包括直立位置测试和刺激测试,也可以补充这些测试并证明 EGJ 阻塞的证据。做出诊断后,内窥镜检查应该是排除解剖学原因(如果尚未进行)的第一步。影像学研究可以识别浸润性病变,但报告的诊断率相对较低。EGJOO 的管理取决于潜在的病因。伴有流出道梗阻的持续吞咽困难的功能性 EGJOO 患者可能需要 EGJ 中断治疗。包括直立位测试和刺激测试,也可以补充这些测试并证明 EGJ 阻塞的证据。做出诊断后,内窥镜检查应该是排除解剖学原因(如果尚未进行)的第一步。影像学研究可以识别浸润性病变,但报告的诊断率相对较低。EGJOO 的管理取决于潜在的病因。伴有流出道梗阻的持续吞咽困难的功能性 EGJOO 患者可能需要 EGJ 中断治疗。但报告的诊断率相对较低。EGJOO 的管理取决于潜在的病因。伴有流出道梗阻的持续吞咽困难的功能性 EGJOO 患者可能需要 EGJ 中断治疗。但报告的诊断率相对较低。EGJOO 的管理取决于潜在的病因。伴有流出道梗阻的持续吞咽困难的功能性 EGJOO 患者可能需要 EGJ 中断治疗。



























 京公网安备 11010802027423号
京公网安备 11010802027423号