当前位置:
X-MOL 学术
›
Adv. Mater.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Engineered PD-L1-Expressing Platelets Reverse New-Onset Type 1 Diabetes.
Advanced Materials ( IF 29.4 ) Pub Date : 2020-05-25 , DOI: 10.1002/adma.201907692 Xudong Zhang 1, 2 , Yang Kang 1, 2 , Jinqiang Wang 1, 2 , Junjie Yan 3 , Qian Chen 1, 2, 4 , Hao Cheng 5 , Peng Huang 6 , Zhen Gu 1, 2, 7, 8
Advanced Materials ( IF 29.4 ) Pub Date : 2020-05-25 , DOI: 10.1002/adma.201907692 Xudong Zhang 1, 2 , Yang Kang 1, 2 , Jinqiang Wang 1, 2 , Junjie Yan 3 , Qian Chen 1, 2, 4 , Hao Cheng 5 , Peng Huang 6 , Zhen Gu 1, 2, 7, 8
Affiliation
|
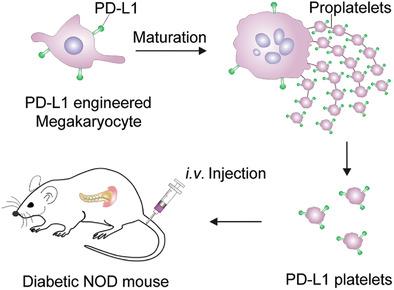
The pathogenesis of Type 1 diabetes (T1D) arises from the destruction of insulin‐producing β‐cells by islet‐specific autoreactive T cells. Inhibition of islet‐specific autoreactive T cells to rescue β‐cells is a promising approach to treat new‐onset T1D. The immune checkpoint signal axis programmed death‐1/programmed death‐ligand 1 (PD‐1/PD‐L1) can effectively regulate the activity of T cells and prevent autoimmune attack. Here, megakaryocyte progenitor cells are genetically engineered to overexpress PD‐L1 to produce immunosuppressive platelets. The PD‐L1‐overexpressing platelets (designated PD‐L1 platelets) accumulate in the inflamed pancreas and may suppress the activity of pancreas autoreactive T cells in newly hyperglycemic non‐obese diabetic (NOD) mice, protecting the insulin‐producing β‐cells from destruction. Moreover, PD‐L1 platelet treatment also increases the percentage of the regulatory T cells (Tregs) and maintains immune tolerance in the pancreas. It is demonstrated that the rescue of β‐cells by PD‐L1 platelets can effectively maintain normoglycemia and reverse diabetes in newly hyperglycemic NOD mice.
中文翻译:

工程化表达PD-L1的血小板可逆转新发1型糖尿病。
1型糖尿病(T1D)的发病机制是由胰岛特异性自身反应性T细胞破坏了产生胰岛素的β细胞引起的。抑制胰岛特异性自身反应性T细胞抢救β细胞是一种治疗新发T1D的有前途的方法。免疫检查点信号轴编程的死亡-1 /编程的死亡配体1(PD-1 / PD-L1)可以有效调节T细胞的活性并预防自身免疫攻击。在这里,巨核细胞祖细胞经过基因工程改造以过表达PD-L1以产生免疫抑制血小板。过表达PD‐L1的血小板(称为PD‐L1血小板)在发炎的胰腺中蓄积,并可能抑制新生的高血糖非肥胖糖尿病(NOD)小鼠的胰腺自身反应性T细胞活性,从而保护产生胰岛素的β细胞免受破坏。此外,PD‐L1血小板治疗还可以增加调节性T细胞(Tregs)的百分比,并维持胰腺的免疫耐受性。事实证明,PD-L1血小板挽救β细胞可以有效维持新血糖过高的NOD小鼠的正常血糖水平并逆转糖尿病。
更新日期:2020-07-01
中文翻译:

工程化表达PD-L1的血小板可逆转新发1型糖尿病。
1型糖尿病(T1D)的发病机制是由胰岛特异性自身反应性T细胞破坏了产生胰岛素的β细胞引起的。抑制胰岛特异性自身反应性T细胞抢救β细胞是一种治疗新发T1D的有前途的方法。免疫检查点信号轴编程的死亡-1 /编程的死亡配体1(PD-1 / PD-L1)可以有效调节T细胞的活性并预防自身免疫攻击。在这里,巨核细胞祖细胞经过基因工程改造以过表达PD-L1以产生免疫抑制血小板。过表达PD‐L1的血小板(称为PD‐L1血小板)在发炎的胰腺中蓄积,并可能抑制新生的高血糖非肥胖糖尿病(NOD)小鼠的胰腺自身反应性T细胞活性,从而保护产生胰岛素的β细胞免受破坏。此外,PD‐L1血小板治疗还可以增加调节性T细胞(Tregs)的百分比,并维持胰腺的免疫耐受性。事实证明,PD-L1血小板挽救β细胞可以有效维持新血糖过高的NOD小鼠的正常血糖水平并逆转糖尿病。



























 京公网安备 11010802027423号
京公网安备 11010802027423号