当前位置:
X-MOL 学术
›
Ann. N. Y. Acad. Sci.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Diagnosis of gastroesophageal reflux: an update on current and emerging modalities
Annals of the New York Academy of Sciences ( IF 5.2 ) Pub Date : 2020-05-19 , DOI: 10.1111/nyas.14369 Daphne Ang 1 , Yeong-Yeh Lee 2, 3, 4 , John O Clarke 5 , Kristle Lynch 6 , Alexandra Guillaume 7 , Frances Onyimba 8 , Afrin Kamal 5 , C Prakash Gyawali 9
Annals of the New York Academy of Sciences ( IF 5.2 ) Pub Date : 2020-05-19 , DOI: 10.1111/nyas.14369 Daphne Ang 1 , Yeong-Yeh Lee 2, 3, 4 , John O Clarke 5 , Kristle Lynch 6 , Alexandra Guillaume 7 , Frances Onyimba 8 , Afrin Kamal 5 , C Prakash Gyawali 9
Affiliation
|
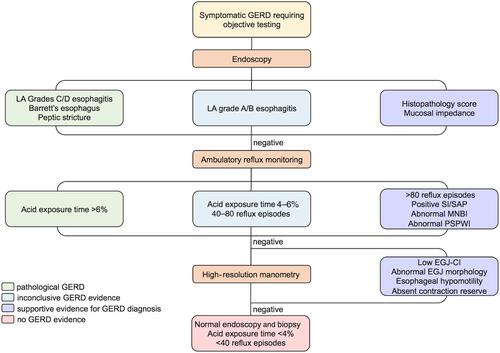
Gastroesophageal reflux disease (GERD) is a common condition characterized by troublesome symptoms or esophageal mucosal lesions attributed to excessive esophageal acid exposure. Various pathophysiological mechanisms account for GERD, including impaired esophageal peristalsis and anatomical or physiological defects at the esophagogastric junction (EGJ). Endoscopy identifies GERD complications and detects potential alternative diagnoses. However, if symptoms persist despite proton pump inhibitor therapy, functional esophageal tests are useful to characterize reflux burden and define the symptom association profile. Ambulatory pH or pH‐impedance monitoring measures the 24‐h acid exposure time, which remains the most reproducible reflux metric and predicts response to antireflux therapy. Apart from identifying peristaltic dysfunction, esophageal high‐resolution manometry defines the morphology and contractile vigor (EGJ‐CI) of the EGJ. Novel metrics obtained from pH‐impedance monitoring include the postreflux swallow–induced peristaltic wave index and mean nocturnal baseline impedance, which augment the diagnostic value of pH‐impedance testing. Mucosal impedance can also be recorded using a probe inserted through a gastroscope, or a novel balloon catheter with arrays of impedance electrodes inserted following sedated endoscopy. The latest developments in functional esophageal tests define the GERD phenotype based on pathogenesis, reflux exposure, structural or motility disorders, and symptom burden, facilitating appropriate treatment.
中文翻译:

胃食管反流的诊断:当前和新兴方式的更新
胃食管反流病 (GERD) 是一种常见疾病,其特征是由于过度暴露于食道酸而引起的不适症状或食道黏膜病变。GERD 的病理生理机制多种多样,包括食管蠕动受损和食管胃交界处 (EGJ) 的解剖或生理缺陷。内窥镜检查可识别 GERD 并发症并检测潜在的替代诊断。然而,如果质子泵抑制剂治疗后症状持续存在,功能性食管检查可用于表征反流负担并确定症状关联特征。动态 pH 值或 pH 阻抗监测测量 24 小时酸暴露时间,这仍然是最可重复的反流指标,并预测对抗反流治疗的反应。除了识别蠕动功能障碍,食管高分辨率测压定义了 EGJ 的形态和收缩力 (EGJ-CI)。从 pH 阻抗监测中获得的新指标包括反流后吞咽诱导的蠕动波指数和平均夜间基线阻抗,它们增加了 pH 阻抗测试的诊断价值。还可以使用通过胃镜插入的探针或在镇静内窥镜检查后插入阻抗电极阵列的新型球囊导管来记录粘膜阻抗。功能性食管检查的最新进展根据发病机制、反流暴露、结构或运动障碍以及症状负担来定义 GERD 表型,从而促进适当的治疗。从 pH 阻抗监测中获得的新指标包括反流后吞咽诱导的蠕动波指数和平均夜间基线阻抗,它们增加了 pH 阻抗测试的诊断价值。还可以使用通过胃镜插入的探针或在镇静内窥镜检查后插入阻抗电极阵列的新型球囊导管来记录粘膜阻抗。功能性食管检查的最新进展根据发病机制、反流暴露、结构或运动障碍以及症状负担来定义 GERD 表型,从而促进适当的治疗。从 pH 阻抗监测中获得的新指标包括反流后吞咽诱导的蠕动波指数和平均夜间基线阻抗,它们增加了 pH 阻抗测试的诊断价值。还可以使用通过胃镜插入的探针或在镇静内窥镜检查后插入阻抗电极阵列的新型球囊导管来记录粘膜阻抗。功能性食管检查的最新进展根据发病机制、反流暴露、结构或运动障碍以及症状负担来定义 GERD 表型,从而促进适当的治疗。或在镇静内窥镜检查后插入阻抗电极阵列的新型球囊导管。功能性食管检查的最新进展根据发病机制、反流暴露、结构或运动障碍以及症状负担来定义 GERD 表型,从而促进适当的治疗。或在镇静内窥镜检查后插入阻抗电极阵列的新型球囊导管。功能性食管检查的最新进展根据发病机制、反流暴露、结构或运动障碍以及症状负担来定义 GERD 表型,从而促进适当的治疗。
更新日期:2020-05-19
中文翻译:

胃食管反流的诊断:当前和新兴方式的更新
胃食管反流病 (GERD) 是一种常见疾病,其特征是由于过度暴露于食道酸而引起的不适症状或食道黏膜病变。GERD 的病理生理机制多种多样,包括食管蠕动受损和食管胃交界处 (EGJ) 的解剖或生理缺陷。内窥镜检查可识别 GERD 并发症并检测潜在的替代诊断。然而,如果质子泵抑制剂治疗后症状持续存在,功能性食管检查可用于表征反流负担并确定症状关联特征。动态 pH 值或 pH 阻抗监测测量 24 小时酸暴露时间,这仍然是最可重复的反流指标,并预测对抗反流治疗的反应。除了识别蠕动功能障碍,食管高分辨率测压定义了 EGJ 的形态和收缩力 (EGJ-CI)。从 pH 阻抗监测中获得的新指标包括反流后吞咽诱导的蠕动波指数和平均夜间基线阻抗,它们增加了 pH 阻抗测试的诊断价值。还可以使用通过胃镜插入的探针或在镇静内窥镜检查后插入阻抗电极阵列的新型球囊导管来记录粘膜阻抗。功能性食管检查的最新进展根据发病机制、反流暴露、结构或运动障碍以及症状负担来定义 GERD 表型,从而促进适当的治疗。从 pH 阻抗监测中获得的新指标包括反流后吞咽诱导的蠕动波指数和平均夜间基线阻抗,它们增加了 pH 阻抗测试的诊断价值。还可以使用通过胃镜插入的探针或在镇静内窥镜检查后插入阻抗电极阵列的新型球囊导管来记录粘膜阻抗。功能性食管检查的最新进展根据发病机制、反流暴露、结构或运动障碍以及症状负担来定义 GERD 表型,从而促进适当的治疗。从 pH 阻抗监测中获得的新指标包括反流后吞咽诱导的蠕动波指数和平均夜间基线阻抗,它们增加了 pH 阻抗测试的诊断价值。还可以使用通过胃镜插入的探针或在镇静内窥镜检查后插入阻抗电极阵列的新型球囊导管来记录粘膜阻抗。功能性食管检查的最新进展根据发病机制、反流暴露、结构或运动障碍以及症状负担来定义 GERD 表型,从而促进适当的治疗。或在镇静内窥镜检查后插入阻抗电极阵列的新型球囊导管。功能性食管检查的最新进展根据发病机制、反流暴露、结构或运动障碍以及症状负担来定义 GERD 表型,从而促进适当的治疗。或在镇静内窥镜检查后插入阻抗电极阵列的新型球囊导管。功能性食管检查的最新进展根据发病机制、反流暴露、结构或运动障碍以及症状负担来定义 GERD 表型,从而促进适当的治疗。


























 京公网安备 11010802027423号
京公网安备 11010802027423号