Regenerative Therapy ( IF 4.3 ) Pub Date : 2020-05-15 , DOI: 10.1016/j.reth.2020.03.012 Takayuki Watanabe 1 , Atsunori Tsuchiya 1 , Suguru Takeuchi 1 , Shunsuke Nojiri 1 , Tomoaki Yoshida 1 , Masahiro Ogawa 1 , Michiko Itoh 2 , Masaaki Takamura 1 , Takayoshi Suganami 3 , Yoshihiro Ogawa 4 , Shuji Terai 1
|
Introduction
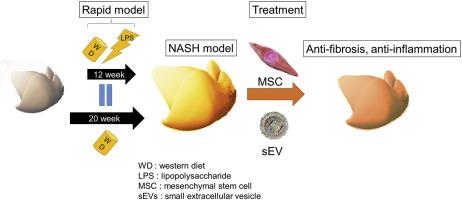
Currently, there are no approved drugs for treating non-alcoholic steatohepatitis (NASH); however, mesenchymal stem cells (MSCs) and their small extracellular vesicles (sEVs), which possess immunomodulatory activities, are potential candidates. This study aimed to develop a mouse model of NASH with rapid accumulation of fibrosis using the pre-established melanocortin type-4 receptor knockout (Mc4r-KO) NASH mouse model and lipopolysaccharide (LPS), and to evaluate the therapeutic effect of MSCs and their sEVs.
Methods
Mc4r-KO mice (8 weeks old, male) were fed a western diet (WD) for 8 weeks. Next, the mice were intraperitoneally injected with lipopolysaccharide (LPS) twice a week for 4 weeks while continuing the WD. To confirm the therapeutic effect of MSCs and sEVs, human adipose tissue-derived MSCs or their sEVs were administered 12 weeks after initiation of the WD, and serum testing, quantitative analysis of fibrosis, and quantitative reverse transcription-polymerase chain reaction qRT-PCR were performed.
Results
By providing a WD combined with LPS treatment, we successfully developed a NASH model with rapid accumulation of fibrosis. Both human MSCs and their sEVs decreased serum alanine transaminase levels and inflammatory markers based on qRT-PCR. Histological analysis showed that MSC or sEV treatment did not affect fat accumulation. However, an improvement in fibrosis in the groups treated with MSCs and their sEVs was observed. Furthermore, after administering MSCs and sEVs, there was a significant increase in anti-inflammatory macrophages in the liver.
Conclusion
We successfully developed a NASH model with rapid accumulation of fibrosis and confirmed the anti-inflammatory and anti-fibrotic effects of MSCs and their sEVs, which may be options for future therapy.
中文翻译:

开发一种具有快速纤维化积累的非酒精性脂肪性肝炎模型,并使用间充质干细胞及其小细胞外囊泡对其进行治疗。
介绍
目前,尚无批准用于治疗非酒精性脂肪性肝炎(NASH)的药物;然而,具有免疫调节活性的间充质干细胞 (MSCs) 及其小细胞外囊泡 (sEVs) 是潜在的候选者。本研究旨在利用预先建立的 4 型黑皮质素受体敲除 ( Mc4r -KO) NASH 小鼠模型和脂多糖 (LPS) 建立快速积聚纤维化的 NASH 小鼠模型,并评估 MSCs 及其治疗效果。电动汽车。
方法
Mc4r -KO 小鼠(8 周大,雄性)喂食西方饮食(WD)8 周。接下来,在继续 WD 的同时,每周两次向小鼠腹膜内注射脂多糖 (LPS),持续 4 周。为确认 MSCs 和 sEVs 的治疗效果,在 WD 开始 12 周后给予人脂肪组织来源的 MSCs 或其 sEVs,并进行血清检测、纤维化定量分析和定量逆转录聚合酶链反应 qRT-PCR执行。
结果
通过提供 WD 与 LPS 治疗相结合,我们成功开发了一种纤维化快速积累的 NASH 模型。基于 qRT-PCR,人类 MSC 及其 sEV 均降低了血清丙氨酸转氨酶水平和炎症标志物。组织学分析表明,MSC 或 sEV 治疗不影响脂肪堆积。然而,观察到用 MSCs 及其 sEVs 治疗的组的纤维化有所改善。此外,在施用 MSCs 和 sEVs 后,肝脏中的抗炎巨噬细胞显着增加。
结论
我们成功开发了一种纤维化快速积累的 NASH 模型,并证实了 MSCs 及其 sEVs 的抗炎和抗纤维化作用,这可能是未来治疗的选择。



























 京公网安备 11010802027423号
京公网安备 11010802027423号