当前位置:
X-MOL 学术
›
Biotechnol. J.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
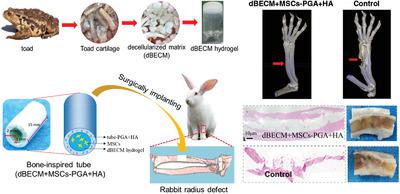
Bone-Inspired Tube Filling Decellularized Matrix of Toad Cartilage Provided an Osteoinductive Microenvironment for Mesenchymal Stem Cells to Facilitate the Radius Defect Repair of Rabbit.
Biotechnology Journal ( IF 4.7 ) Pub Date : 2020-04-30 , DOI: 10.1002/biot.202000004 He-Lin Xu 1 , Wai-Geng Yang 1 , Pian-Pian Chen 1 , Rui Chen 1 , Peng-Peng Xue 1 , Li-Fen Wang 1 , Jian-Dong Yuan 2 , Qing Yao 1 , Bin Chen 3 , Ying-Zheng Zhao 1
Biotechnology Journal ( IF 4.7 ) Pub Date : 2020-04-30 , DOI: 10.1002/biot.202000004 He-Lin Xu 1 , Wai-Geng Yang 1 , Pian-Pian Chen 1 , Rui Chen 1 , Peng-Peng Xue 1 , Li-Fen Wang 1 , Jian-Dong Yuan 2 , Qing Yao 1 , Bin Chen 3 , Ying-Zheng Zhao 1
Affiliation
|
Toad bone not only contains the rich cartilage‐like matrix but also presents low immunogenicity. It is inferred that decellularized toad bone matrix (dBECM) may provide the more profitable osteoinductive microenvironment for mesenchymal stem cells (MSCs) to promote the repair of bone defects. Herein, a hollow bone‐inspired tube is first made from hydroxyapatite (HA) and poly (γ‐glutamic acid) (PGA), and then MSCs/dBECM hydrogel is uniformly filled to its central cavity, constructing a biomimetic bone (dBECM + MSCs − PGA + HA). In vitro scratch and transwell experiments show that dBECM hydrogel not only effectively promotes migration and proliferation of MSCs but also induces their osteogenic differentiation. Moreover, the less inflammatory macrophages infiltrate at rat skin after subcutaneously injecting dBECM hydrogel, indicating its low potential for inflammatory attack. After implanting dBECM + MSCs − PGA + HA to critical radius defect of rabbit, X‐ray and CT imaging shows that the cortex is effectively regenerated and the medullary cavity recanalization is completed at 20 weeks. Moreover, the expression of Collagen‐II and OCN are obviously increased in the defect after implanting dBECM + MSCs − PGA + HA. The therapeutic mechanism of dBECM + MSCs − PGA + HA scaffold are highly associated with the enhanced angiogenesis. Collectively, the biomimetic dBECM + MSCs − PGA + HA scaffold may be a promising strategy to improve radius defect healing efficiency.
中文翻译:

蟾蜍骨骨管填充脱细胞基质为间充质干细胞提供了骨诱导微环境,以促进兔the骨缺损的修复。
蟾蜍骨不仅包含丰富的软骨样基质,而且免疫原性低。可以推断,脱细胞的蟾蜍骨基质(dBECM)可能为间充质干细胞(MSC)提供更有利可图的骨诱导微环境,以促进骨缺损的修复。在此,首先用羟基磷灰石(HA)和聚(γ-谷氨酸)(PGA)制成空心骨启发管,然后将MSCs / dBECM水凝胶均匀地填充到其中央腔中,从而构建仿生骨骼(dBECM + MSCs) -PGA + HA)。体外划痕和穿孔实验表明,dBECM水凝胶不仅有效地促进了MSC的迁移和增殖,还诱导了它们的成骨分化。此外,皮下注射dBECM水凝胶后,炎症较少的巨噬细胞会在大鼠皮肤中浸润,说明其发炎性攻击的可能性较低。将dBECM + MSCs-PGA + HA植入兔的radius骨严重缺损后,X射线和CT成像显示皮层得到了有效的再生,髓腔的再通在20周后完成。此外,植入dBECM + MSCs-PGA + HA后,缺损中胶原II和OCN的表达明显增加。dBECM + MSCs-PGA + HA支架的治疗机制与增强的血管生成高度相关。总的来说,仿生的dBECM + MSCs-PGA + HA支架可能是提高radius骨缺损愈合效率的有前途的策略。X射线和CT成像显示皮层得到了有效的再生,髓腔再通在20周后完成。此外,植入dBECM + MSCs-PGA + HA后,缺损中胶原II和OCN的表达明显增加。dBECM + MSCs-PGA + HA支架的治疗机制与增强的血管生成高度相关。总的来说,仿生的dBECM + MSCs-PGA + HA支架可能是提高radius骨缺损愈合效率的有前途的策略。X射线和CT成像显示皮层得到了有效的再生,髓腔再通在20周后完成。此外,植入dBECM + MSCs-PGA + HA后,缺损中胶原II和OCN的表达明显增加。dBECM + MSCs-PGA + HA支架的治疗机制与增强的血管生成高度相关。总的来说,仿生的dBECM + MSCs-PGA + HA支架可能是提高radius骨缺损愈合效率的有前途的策略。
更新日期:2020-04-30
中文翻译:

蟾蜍骨骨管填充脱细胞基质为间充质干细胞提供了骨诱导微环境,以促进兔the骨缺损的修复。
蟾蜍骨不仅包含丰富的软骨样基质,而且免疫原性低。可以推断,脱细胞的蟾蜍骨基质(dBECM)可能为间充质干细胞(MSC)提供更有利可图的骨诱导微环境,以促进骨缺损的修复。在此,首先用羟基磷灰石(HA)和聚(γ-谷氨酸)(PGA)制成空心骨启发管,然后将MSCs / dBECM水凝胶均匀地填充到其中央腔中,从而构建仿生骨骼(dBECM + MSCs) -PGA + HA)。体外划痕和穿孔实验表明,dBECM水凝胶不仅有效地促进了MSC的迁移和增殖,还诱导了它们的成骨分化。此外,皮下注射dBECM水凝胶后,炎症较少的巨噬细胞会在大鼠皮肤中浸润,说明其发炎性攻击的可能性较低。将dBECM + MSCs-PGA + HA植入兔的radius骨严重缺损后,X射线和CT成像显示皮层得到了有效的再生,髓腔的再通在20周后完成。此外,植入dBECM + MSCs-PGA + HA后,缺损中胶原II和OCN的表达明显增加。dBECM + MSCs-PGA + HA支架的治疗机制与增强的血管生成高度相关。总的来说,仿生的dBECM + MSCs-PGA + HA支架可能是提高radius骨缺损愈合效率的有前途的策略。X射线和CT成像显示皮层得到了有效的再生,髓腔再通在20周后完成。此外,植入dBECM + MSCs-PGA + HA后,缺损中胶原II和OCN的表达明显增加。dBECM + MSCs-PGA + HA支架的治疗机制与增强的血管生成高度相关。总的来说,仿生的dBECM + MSCs-PGA + HA支架可能是提高radius骨缺损愈合效率的有前途的策略。X射线和CT成像显示皮层得到了有效的再生,髓腔再通在20周后完成。此外,植入dBECM + MSCs-PGA + HA后,缺损中胶原II和OCN的表达明显增加。dBECM + MSCs-PGA + HA支架的治疗机制与增强的血管生成高度相关。总的来说,仿生的dBECM + MSCs-PGA + HA支架可能是提高radius骨缺损愈合效率的有前途的策略。


























 京公网安备 11010802027423号
京公网安备 11010802027423号