Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Tumour cell PD-L1 expression is prognostic in patients with malignant pleural effusion: the impact of C-reactive protein and immune-checkpoint inhibition.
Scientific Reports ( IF 4.6 ) Pub Date : 2020-04-01 , DOI: 10.1038/s41598-020-62813-2 Bahil Ghanim 1, 2 , Anna Rosenmayr 1 , Paul Stockhammer 3, 4 , Melanie Vogl 1, 2 , Ali Celik 5 , Aynur Bas 5 , Ismail Cuneyt Kurul 5 , Nalan Akyurek 6 , Alexander Varga 7 , Till Plönes 3 , Agnes Bankfalvi 8 , Thomas Hager 8 , Martin Schuler 9 , Klaus Hackner 10 , Peter Errhalt 10 , Axel Scheed 1, 2 , Gernot Seebacher 1, 2 , Balazs Hegedus 3 , Elisabeth Stubenberger 1, 2 , Clemens Aigner 3
Scientific Reports ( IF 4.6 ) Pub Date : 2020-04-01 , DOI: 10.1038/s41598-020-62813-2 Bahil Ghanim 1, 2 , Anna Rosenmayr 1 , Paul Stockhammer 3, 4 , Melanie Vogl 1, 2 , Ali Celik 5 , Aynur Bas 5 , Ismail Cuneyt Kurul 5 , Nalan Akyurek 6 , Alexander Varga 7 , Till Plönes 3 , Agnes Bankfalvi 8 , Thomas Hager 8 , Martin Schuler 9 , Klaus Hackner 10 , Peter Errhalt 10 , Axel Scheed 1, 2 , Gernot Seebacher 1, 2 , Balazs Hegedus 3 , Elisabeth Stubenberger 1, 2 , Clemens Aigner 3
Affiliation
|
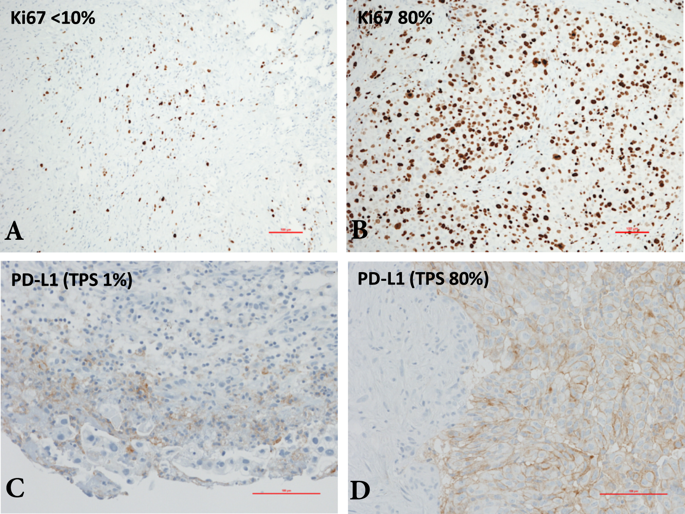
Malignant pleural effusion (MPE) confers dismal prognosis and has limited treatment options. While immune-checkpoint inhibition (ICI) proved clinical efficacy in a variety of malignancies, data on the prognostic role of PD-L1 in MPE is scarce. We retrospectively studied PD-L1 tumour proportion score and Ki-67 index in pleural biopsies or cytologies from 123 patients (69 lung cancer, 25 mesothelioma, and 29 extrathoracic primary malignancies). Additionally, the impact of C-reactive protein (CRP) and platelet count was also analysed. Median overall survival (OS) after MPE diagnosis was 9 months. Patients with PD-L1 positive tumours (≥1%) had significantly shorter OS than patients with negative PD-L1 status (p = 0.031). CRP and Ki-67 index were also prognostic and remained independent prognosticators after multivariate analysis. Interestingly, Ki-67 index and CRP influenced the prognostic power of PD-L1. Finally, patients receiving ICI tended to have a longer median OS and CRP - but not PD-L1 - was a significant prognosticator in this subgroup. In summary, histological and circulating biomarkers should also be taken into account as potential biomarkers in ICI therapy and they may have an impact on the prognostic power of PD-L1. Our findings might help personalizing immune-checkpoint inhibition for patients with MPE and warrant further prospective validation.
中文翻译:

恶性胸腔积液患者的肿瘤细胞PD-L1表达是预后的:C反应蛋白和免疫检查点抑制的影响。
恶性胸腔积液(MPE)可使预后不良,治疗选择有限。尽管免疫检查点抑制(ICI)在多种恶性肿瘤中均证明了临床疗效,但有关PD-L1在MPE中的预后作用的数据却很少。我们回顾性研究了123例患者(69例肺癌,25例间皮瘤和29例胸外原发性恶性肿瘤)的胸膜活检或细胞学检查中PD-L1肿瘤比例评分和Ki-67指数。此外,还分析了C反应蛋白(CRP)和血小板计数的影响。MPE诊断后的中位总生存期(OS)为9个月。PD-L1阳性肿瘤(≥1%)的患者的OS明显短于PD-L1阴性患者(p = 0.031)。CRP和Ki-67指数也具有预后性,在进行多变量分析后仍保持独立的预后。有趣的是 Ki-67指数和CRP影响PD-L1的预后。最后,接受ICI的患者倾向于具有更长的中位OS和CRP,而PD-L1没有,是该亚组的重要预后指标。总之,组织学和循环生物标志物也应考虑作为ICI治疗中的潜在生物标志物,它们可能对PD-L1的预后影响。我们的发现可能有助于个性化MPE患者的免疫检查点抑制作用,并有待进一步的前瞻性验证。组织学和循环生物标志物也应被视为ICI治疗中的潜在生物标志物,它们可能对PD-L1的预后能力产生影响。我们的发现可能有助于个性化MPE患者的免疫检查点抑制作用,并有待进一步的前瞻性验证。组织学和循环生物标志物也应被视为ICI治疗中的潜在生物标志物,它们可能对PD-L1的预后能力产生影响。我们的发现可能有助于个性化MPE患者的免疫检查点抑制作用,并有待进一步的前瞻性验证。
更新日期:2020-04-01
中文翻译:

恶性胸腔积液患者的肿瘤细胞PD-L1表达是预后的:C反应蛋白和免疫检查点抑制的影响。
恶性胸腔积液(MPE)可使预后不良,治疗选择有限。尽管免疫检查点抑制(ICI)在多种恶性肿瘤中均证明了临床疗效,但有关PD-L1在MPE中的预后作用的数据却很少。我们回顾性研究了123例患者(69例肺癌,25例间皮瘤和29例胸外原发性恶性肿瘤)的胸膜活检或细胞学检查中PD-L1肿瘤比例评分和Ki-67指数。此外,还分析了C反应蛋白(CRP)和血小板计数的影响。MPE诊断后的中位总生存期(OS)为9个月。PD-L1阳性肿瘤(≥1%)的患者的OS明显短于PD-L1阴性患者(p = 0.031)。CRP和Ki-67指数也具有预后性,在进行多变量分析后仍保持独立的预后。有趣的是 Ki-67指数和CRP影响PD-L1的预后。最后,接受ICI的患者倾向于具有更长的中位OS和CRP,而PD-L1没有,是该亚组的重要预后指标。总之,组织学和循环生物标志物也应考虑作为ICI治疗中的潜在生物标志物,它们可能对PD-L1的预后影响。我们的发现可能有助于个性化MPE患者的免疫检查点抑制作用,并有待进一步的前瞻性验证。组织学和循环生物标志物也应被视为ICI治疗中的潜在生物标志物,它们可能对PD-L1的预后能力产生影响。我们的发现可能有助于个性化MPE患者的免疫检查点抑制作用,并有待进一步的前瞻性验证。组织学和循环生物标志物也应被视为ICI治疗中的潜在生物标志物,它们可能对PD-L1的预后能力产生影响。我们的发现可能有助于个性化MPE患者的免疫检查点抑制作用,并有待进一步的前瞻性验证。


























 京公网安备 11010802027423号
京公网安备 11010802027423号