Scientific Reports ( IF 4.6 ) Pub Date : 2020-03-27 , DOI: 10.1038/s41598-020-62087-8 Stefan J Grau 1 , Mario Löhr 2 , Valeria Taurisano 3 , Herbert Trautner 4 , Marco Timmer 1 , Stephanie G Schwab 1 , Jürgen Hampl 1 , Thorsten Annecke 3
|
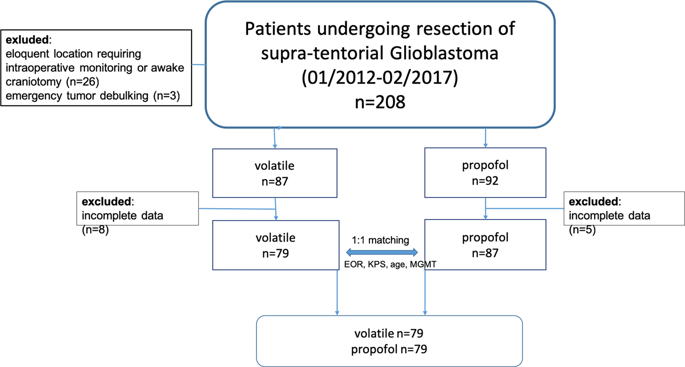
Anaesthetics used during cancer surgery may influence tumour cells and immunological response. The aim of this study was to evaluate a potential influence of the anaesthetic method (inhaled anaesthetics versus total-intravenous anaesthesia using propofol) on recurrence-free and overall survival in glioblastoma patients. We retrospectively identified patients undergoing resection of contrast enhancing glioblastoma under general anaesthesia followed by standard adjuvant treatment between January 2010 and February 2017 at two University Hospitals. Matched pairs of patients receiving either balanced with volatile anaesthetics or total intravenous anaesthesia were generated according to the known prognostic factors (extent of resection, methyl-guanine-methyl-transferase (MGMT) promoter methylation, age, Karnofsky performance score). Groups were compared using chi-square and Whitney-Man-U test. Time to recurrence was calculated using Kaplan Meier estimates. Log Rank test was used to assess the influence of the anaesthetic method. One hundred and fifty-eight (79:79) patients were included. Groups showed no significant difference in recurrence-free (volatiles: 8.0 (95% CI 6.5–9.8) vs. propofol: 8.4 (95% CI 7.9–10.1) months; p = 0.54) or overall survival (propofol: 17.4 (95% CI 14.0–20.7) vs. volatiles: 16.9 (95% CI 13.9–20.1) months; p = 0.85). In contrast to potential beneficial effects in some other solid tumours, the choice of anaesthetic method had no impact on survival in patients with glioblastoma in a well-defined cohort.
中文翻译:

胶质母细胞瘤手术的麻醉选择不会影响复发时间。
癌症手术中使用的麻醉剂可能会影响肿瘤细胞和免疫反应。这项研究的目的是评估麻醉方法(吸入麻醉与异丙酚全静脉麻醉)对成胶质细胞瘤患者无复发生存和总体生存的潜在影响。我们回顾性确定了在2010年1月至2017年2月期间在两家大学医院接受全麻切除对比增强胶质母细胞瘤的患者,然后接受标准辅助治疗。根据已知的预后因素(切除范围,甲基鸟嘌呤甲基转移酶(MGMT)启动子甲基化,年龄,卡诺夫斯基功能评分),生成了接受挥发性麻醉剂或全静脉麻醉平衡的患者配对。使用卡方检验和惠特尼-曼-U检验比较各组。使用Kaplan Meier估计值计算复发时间。使用Log Rank检验评估麻醉方法的影响。包括一百八十五(79:79)患者。各组的无复发(挥发物:8.0(95%CI 6.5–9.8)与丙泊酚:8.4(95%CI 7.9-10.1)个月; p = 0.54)或总生存率(丙泊酚:17.4(95%) CI 14.0–20.7)与挥发分:16.9(95%CI 13.9–20.1)个月; p = 0.85)。与某些其他实体瘤的潜在有益作用相反,在定义明确的队列中,选择麻醉方法对胶质母细胞瘤患者的生存没有影响。使用Log Rank检验评估麻醉方法的影响。包括一百八十五(79:79)患者。各组的无复发(挥发物:8.0(95%CI 6.5–9.8)与丙泊酚:8.4(95%CI 7.9-10.1)个月; p = 0.54)或总生存率(丙泊酚:17.4(95%) CI 14.0–20.7)与挥发分:16.9(95%CI 13.9–20.1)个月; p = 0.85)。与某些其他实体瘤的潜在有益作用相反,在定义明确的队列中,选择麻醉方法对胶质母细胞瘤患者的生存没有影响。使用Log Rank检验评估麻醉方法的影响。包括一百八十五(79:79)患者。各组的无复发(挥发物:8.0(95%CI 6.5–9.8)与丙泊酚:8.4(95%CI 7.9-10.1)个月; p = 0.54)或总生存率(丙泊酚:17.4(95%) CI 14.0–20.7)与挥发分:16.9(95%CI 13.9–20.1)个月; p = 0.85)。与某些其他实体瘤的潜在有益作用相反,在定义明确的队列中,选择麻醉方法对胶质母细胞瘤患者的生存没有影响。4(95%CI 14.0–20.7)与挥发分:16.9(95%CI 13.9–20.1)月;p = 0.85)。与某些其他实体瘤的潜在有益作用相反,在定义明确的队列中,选择麻醉方法对胶质母细胞瘤患者的生存没有影响。4(95%CI 14.0–20.7)与挥发分:16.9(95%CI 13.9–20.1);p = 0.85)。与某些其他实体瘤的潜在有益作用相反,在定义明确的队列中,选择麻醉方法对胶质母细胞瘤患者的生存没有影响。


























 京公网安备 11010802027423号
京公网安备 11010802027423号