PLOS Medicine ( IF 15.8 ) Pub Date : 2020-03-17 , DOI: 10.1371/journal.pmed.1003061 Maryam Mozooni 1 , Craig E Pennell 2 , David B Preen 1
|
Background
Migrant women, especially from Indian and African ethnicity, have a higher risk of stillbirth than native-born populations in high-income countries. Differential access or timing of ANC and the uptake of other services may play a role. We investigated the pattern of healthcare utilisation among migrant women and its relationship with the risk of stillbirth (SB)—antepartum stillbirth (AnteSB) and intrapartum stillbirth (IntraSB)—in Western Australia (WA).
Methods and findings
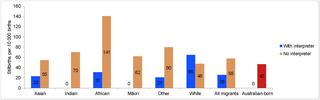
A retrospective cohort study using de-identified linked data from perinatal, birth, death, hospital, and birth defects registrations through the WA Data Linkage System was undertaken. All (N = 260,997) non-Indigenous births (2005–2013) were included. Logistic regression analysis was used to estimate odds ratios and 95% CI for AnteSB and IntraSB comparing migrant women from white, Asian, Indian, African, Māori, and ‘other’ ethnicities with Australian-born women controlling for risk factors and potential healthcare-related covariates. Of all the births, 66.1% were to Australian-born and 33.9% to migrant women. The mean age (years) was 29.5 among the Australian-born and 30.5 among the migrant mothers. For parity, 42.3% of Australian-born women, 58.2% of Indian women, and 29.3% of African women were nulliparous. Only 5.3% of Māori and 9.2% of African migrants had private health insurance in contrast to 43.1% of Australian-born women. Among Australian-born women, 14% had smoked in pregnancy whereas only 0.7% and 1.9% of migrants from Indian and African backgrounds, respectively, had smoked in pregnancy. The odds of AnteSB was elevated in African (odds ratio [OR] 2.22, 95% CI 1.48–2.13, P < 0.001), Indian (OR 1.64, 95% CI 1.13–2.44, P = 0.013), and other women (OR 1.46, 95% CI 1.07–1.97, P = 0.016) whereas IntraSB was higher in African (OR 5.24, 95% CI 3.22–8.54, P < 0.001) and ‘other’ women (OR 2.18, 95% CI 1.35–3.54, P = 0.002) compared with Australian-born women. When migrants were stratified by timing of first antenatal visit, the odds of AnteSB was exclusively increased in those who commenced ANC later than 14 weeks gestation in women from Indian (OR 2.16, 95% CI 1.18–3.95, P = 0.013), Māori (OR 3.03, 95% CI 1.43–6.45, P = 0.004), and ‘other’ (OR 2.19, 95% CI 1.34–3.58, P = 0.002) ethnicities. With midwife-only intrapartum care, the odds of IntraSB for viable births in African and ‘other’ migrants (combined) were more than 3 times that of Australian-born women (OR 3.43, 95% CI 1.28–9.19, P = 0.014); however, with multidisciplinary intrapartum care, the odds were similar to that of Australian-born group (OR 1.34, 95% CI 0.30–5.98, P = 0.695). Compared with Australian-born women, migrant women who utilised interpreter services had a lower risk of SB (OR 0.51, 95% CI 0.27–0.96, P = 0.035); those who did not utilise interpreters had a higher risk of SB (OR 1.20, 95% CI 1.07–1.35, P < 0.001). Covariates partially available in the data set comprised the main limitation of the study.
Conclusion
Late commencement of ANC, underutilisation of interpreter services, and midwife-only intrapartum care are associated with increased risk of SB in migrant women. Education to improve early engagement with ANC, better uptake of interpreter services, and the provision of multidisciplinary-team intrapartum care to women specifically from African and ‘other’ backgrounds may reduce the risk of SB in migrants.
中文翻译:

西澳大利亚州移民中与产前和产中死产风险相关的医疗保健因素(2005-2013年):一项回顾性队列研究。
背景
与高收入国家的土著人口相比,移徙妇女,特别是印度和非洲种族的妇女,死胎的风险更高。ANC的差异访问或时间安排以及其他服务的使用可能会起到一定作用。我们调查了西澳大利亚州(WA)移民妇女中医疗保健利用的模式及其与死产(SB)(产前死产(AnteSB)和产内死产(IntraSB))的关系。
方法和发现
进行了一项回顾性队列研究,该研究使用了通过WA数据链接系统从围产期,出生,死亡,医院和出生缺陷登记中获得的身份不明的链接数据。全部(N= 260,997)非土著婴儿出生(2005-2013)。使用Logistic回归分析来估计AnteSB和IntraSB的比值比和95%CI,将来自白人,亚洲,印度,非洲,毛利人和“其他”族裔的移民妇女与控制风险因素及与医疗相关的澳大利亚出生妇女进行比较协变量 在所有出生中,澳大利亚出生的占66.1%,移徙妇女的占33.9%。澳大利亚出生的人的平均年龄(岁)为29.5岁,移民母亲的平均年龄(岁)为30.5岁。就平价而言,未出生的澳大利亚妇女占42.3%,印度妇女占58.2%,非洲妇女占29.3%。只有5.3%的毛利人和9.2%的非洲移民有私人健康保险,而在澳大利亚出生的妇女中只有43.1%。在澳大利亚出生的妇女中,有14%的人在怀孕期间吸烟,而只有0.7%和1。来自印度和非洲背景的移民分别有9%在怀孕期间吸烟。非洲人AnteSB的几率有所提高(赔率[OR] 2.22、95%CI 1.48–2.13,P <0.001),印度裔(OR 1.64,95%CI 1.13–2.44,P = 0.013)和其他女性(OR 1.46,95%CI 1.07–1.97,P = 0.016),而非洲的IntraSB较高(OR 5.24,与澳大利亚出生的妇女相比,95%CI 3.22–8.54,P <0.001)和其他女性(OR 2.18,95%CI 1.35–3.54,P = 0.002)。当按首次产前检查的时间对移民进行分层时,来自印度(OR 2.16,95%CI 1.18–3.95,P = 0.013),毛利人的妇女中,刚开始妊娠14周后开始ANC的人群中,AnteSB的可能性会增加。或3.03,95%CI 1.43–6.45,P = 0.004)和“其他”(或2.19,95%CI 1.34–3.58,P= 0.002)种族。在仅进行助产士产期护理的情况下,IntraSB在非洲和其他移民(合并)中活产的几率是澳大利亚出生妇女的三倍以上(OR 3.43,95%CI 1.28-9.19,P = 0.014) ; 然而,在多学科产期护理中,几率与澳大利亚出生的组相似(OR 1.34,95%CI 0.30–5.98,P = 0.695)。与澳大利亚出生的妇女相比,使用口译服务的移徙妇女患SB的风险较低(OR 0.51,95%CI 0.27–0.96,P = 0.035);那些不使用口译员的人患SB的风险更高(OR 1.20,95%CI 1.07-1.35,P <0.001)。数据集中部分可用的协变量构成了研究的主要局限。
结论
ANC的延迟启动,口译服务的未充分利用以及仅助产士的产期护理与移徙妇女罹患SB的风险增加相关。开展教育以改善与ANC的早期接触,更好地接受口译服务以及特别为来自非洲和“其他”背景的妇女提供跨学科团队的产期护理,可能会降低移民中SB的风险。


























 京公网安备 11010802027423号
京公网安备 11010802027423号