The Lancet Respiratory Medicine ( IF 76.2 ) Pub Date : 2020-03-13 , DOI: 10.1016/s2213-2600(19)30397-2 Amin Adibi 1 , Don D Sin 2 , Abdollah Safari 1 , Kate M Johnson 1 , Shawn D Aaron 3 , J Mark FitzGerald 4 , Mohsen Sadatsafavi 5
|
Background
Accurate prediction of exacerbation risk enables personalised care for patients with chronic obstructive pulmonary disease (COPD). We developed and validated a generalisable model to predict individualised rate and severity of COPD exacerbations.
Methods
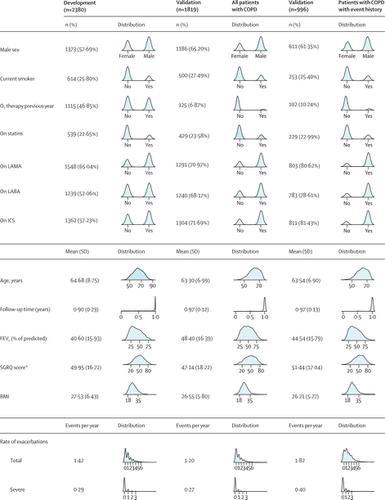
In this risk modelling study, we pooled data from three COPD trials on patients with a history of exacerbations. We developed a mixed-effect model to predict exacerbations over 1 year. Severe exacerbations were those requiring inpatient care. Predictors were history of exacerbations, age, sex, body-mass index, smoking status, domiciliary oxygen therapy, lung function, symptom burden, and current medication use. Evaluation of COPD Longitudinally to Identify Predictive Surrogate End-points (ECLIPSE), a multicentre cohort study, was used for external validation.
Results
The development dataset included 2380 patients, 1373 (58%) of whom were men. Mean age was 64·7 years (SD 8·8). Mean exacerbation rate was 1·42 events per year and 0·29 events per year were severe. When validated against all patients with COPD in ECLIPSE (mean exacerbation rate was 1·20 events per year, 0·27 events per year were severe), the area-under-curve (AUC) was 0·81 (95% CI 0·79–0·83) for at least two exacerbations and 0·77 (95% CI 0·74–0·80) for at least one severe exacerbation. Predicted exacerbation and observed exacerbation rates were similar (1·31 events per year for all exacerbations and 0·25 events per year for severe exacerbations vs 1·20 events per year and 0·27 events per year). In ECLIPSE, in patients with previous exacerbation history (mean exacerbation rate was 1·82 events per year, 0·40 events per year were severe), AUC was 0·73 (95% CI 0·70–0·76) for two or more exacerbations and 0·74 (95% CI 0·70–0·78) for at least one severe exacerbation. Calibration was accurate for severe exacerbations (predicted 0·37 events per year vs observed 0·40 events per year) and all exacerbations (predicted 1·80 events per year vs observed 1·82 events per year).
Interpretation
This model can be used as a decision tool to personalise COPD treatment and prevent exacerbations.
Funding
Canadian Institutes of Health Research.
中文翻译:

慢性阻塞性肺病急性加重预测工具 (ACCEPT):建模研究
背景
准确预测恶化风险可以为慢性阻塞性肺病 (COPD) 患者提供个性化护理。我们开发并验证了一个通用模型来预测 COPD 恶化的个体化发生率和严重程度。
方法
在这项风险模型研究中,我们汇集了三项针对有加重史患者的慢性阻塞性肺病试验的数据。我们开发了一个混合效应模型来预测一年内的病情加重。严重恶化是需要住院治疗的情况。预测因素包括病情加重史、年龄、性别、体重指数、吸烟状况、家庭氧疗、肺功能、症状负担和当前药物使用情况。慢性阻塞性肺病纵向评估以识别预测替代终点 (ECLIPSE) 是一项多中心队列研究,用于外部验证。
结果
开发数据集包括 2380 名患者,其中 1373 名 (58%) 是男性。平均年龄为 64·7 岁 (SD 8·8)。平均恶化率为每年 1·42 起事件,每年 0·29 起严重事件。在 ECLIPSE 中对所有 COPD 患者进行验证时(平均恶化率为每年 1·20 起事件,每年 0·27 起严重事件),曲线下面积 (AUC) 为 0·81 (95% CI 0· 79–0·83) 表示至少两次恶化,0·77 (95% CI 0·74–0·80) 表示至少一次严重恶化。预测的恶化和观察到的恶化率相似(所有恶化每年发生 1·31 起事件,严重恶化每年发生 0·25 起事件,而严重恶化每年发生1·20 起事件和每年 0·27 起事件)。在 ECLIPSE 中,在既往有恶化史的患者中(平均恶化率为每年 1·82 起事件,每年 0·40 起严重事件),两次的 AUC 为 0·73(95% CI 0·70–0·76)或多次恶化,至少一次严重恶化为 0·74 (95% CI 0·70–0·78)。对于严重急性加重(每年预测 0·37 起事件与每年观察到 0·40 起事件)和所有加重(每年预测 1·80 起事件与每年观察到 1·82 起事件),校准是准确的。
解释
该模型可用作个性化 COPD 治疗和预防病情加重的决策工具。
资金
加拿大健康研究所。



























 京公网安备 11010802027423号
京公网安备 11010802027423号