Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Guselkumab in patients with active psoriatic arthritis who were biologic-naive or had previously received TNFα inhibitor treatment (DISCOVER-1): a double-blind, randomised, placebo-controlled phase 3 trial.
The Lancet ( IF 168.9 ) Pub Date : 2020-03-13 , DOI: 10.1016/s0140-6736(20)30265-8 Atul Deodhar 1 , Philip S Helliwell 2 , Wolf-Henning Boehncke 3 , Alexa P Kollmeier 4 , Elizabeth C Hsia 5 , Ramanand A Subramanian 6 , Xie L Xu 4 , Shihong Sheng 7 , Prasheen Agarwal 7 , Bei Zhou 7 , Yanli Zhuang 8 , Christopher T Ritchlin 9 ,
中文翻译:

Guselkumab用于患有活动性银屑病关节炎的患者,如果是初生或曾接受过TNFα抑制剂治疗(DISCOVER-1),则为双盲,随机,安慰剂对照的3期临床试验。
更新日期:2020-04-03
The Lancet ( IF 168.9 ) Pub Date : 2020-03-13 , DOI: 10.1016/s0140-6736(20)30265-8 Atul Deodhar 1 , Philip S Helliwell 2 , Wolf-Henning Boehncke 3 , Alexa P Kollmeier 4 , Elizabeth C Hsia 5 , Ramanand A Subramanian 6 , Xie L Xu 4 , Shihong Sheng 7 , Prasheen Agarwal 7 , Bei Zhou 7 , Yanli Zhuang 8 , Christopher T Ritchlin 9 ,
Affiliation
|
Background
Many patients with psoriatic arthritis have an inadequate response to tumor necrosis factor (TNF) inhibitors. Guselkumab, a specific inhibitor of interleukin-23 (IL-23) via IL-23 p19 subunit binding, significantly improved psoriatic arthritis signs and symptoms with an acceptable safety profile in a phase 2 trial.Methods
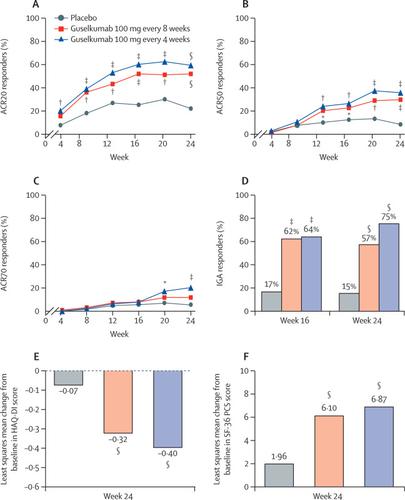
This multicentre, double-blind, randomised, placebo-controlled, phase 3 trial was done at 86 sites in 13 countries across Asia, Australasia, Europe, and North America and enrolled adults with active psoriatic arthritis (at least three swollen and three tender joints; and C-reactive protein ≥0·3 mg/dL) despite standard therapies. Eligibility criteria included inadequate response to or intolerance of standard treatment, including at least 4 months of apremilast, at least 3 months of non-biologic disease-modifying antirheumatic drugs (DMARDs), or at least 4 weeks of non-steroidal anti-inflammatory drugs for psoriatic arthritis. About 30% of study participants could have previously received one or two TNF inhibitors. Patients were randomly assigned (1:1:1, computer-generated permuted blocks; stratified by baseline DMARD and previous TNF inhibitor use) to subcutaneous guselkumab 100 mg every 4 weeks; guselkumab 100 mg at weeks 0, 4, then every 8 weeks; or matching placebo. The primary endpoint was American College of Rheumatology 20% improvement (ACR20) at week 24 in all patients per assigned treatment group using non-responder imputation. Safety was assessed in all patients per treatment received. This trial is registered at , (active, not recruiting).Findings
From Aug 28, 2017, to Aug 17, 2018, we screened 624 patients, of whom 381 were randomly assigned and treated with guselkumab every 4 weeks (n=128), guselkumab every 8 weeks (n=127), or placebo (n=126). 362 patients continued study treatment up to week 24. The primary endpoint was met: ACR20 at week 24 was achieved by significantly greater proportions of patients in the guselkumab every 4 weeks group (76 [59%] of 128 [95% CI 50–68]) and every 8 weeks group (66 [52%] of 127 [43–61]) than in the placebo group (28 [22%] of 126 [15–30]), with percentage differences versus placebo of 37% (95% CI 26–48) for the every 4 weeks group and 30% (19–41) for the every 8 weeks group (both p<0·0001). Serious adverse events up to week 24 occurred in no patients receiving guselkumab every 4 weeks, four (3%) patients receiving guselkumab every 8 weeks, and five (4%) patients receiving placebo. Up to week 24, one patient in the placebo group died from cardiac failure and two had serious infections; no guselkumab-treated patient died or had serious infections.Interpretation
Guselkumab demonstrated a favourable benefit–risk profile and might be an effective treatment option for patients with active psoriatic arthritis.Funding
Janssen Research and Development.中文翻译:

Guselkumab用于患有活动性银屑病关节炎的患者,如果是初生或曾接受过TNFα抑制剂治疗(DISCOVER-1),则为双盲,随机,安慰剂对照的3期临床试验。

























 京公网安备 11010802027423号
京公网安备 11010802027423号