当前位置:
X-MOL 学术
›
Cancer Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Time to diagnostic resolution after an uncertain screening mammogram in an underserved population.
Cancer Medicine ( IF 4 ) Pub Date : 2020-03-11 , DOI: 10.1002/cam4.2970 Anita J Kumar 1, 2 , Darcy Banco 1 , Elise E Steinberger 1 , Joanna Chen 1 , RuthAnn Weidner 1 , Shital Makim 3 , Susan K Parsons 1, 2
Cancer Medicine ( IF 4 ) Pub Date : 2020-03-11 , DOI: 10.1002/cam4.2970 Anita J Kumar 1, 2 , Darcy Banco 1 , Elise E Steinberger 1 , Joanna Chen 1 , RuthAnn Weidner 1 , Shital Makim 3 , Susan K Parsons 1, 2
Affiliation
|
BACKGROUND
Screening mammography has reduced breast cancer-associated mortality worldwide. Approximately 10% of patients require further diagnostic testing after an uncertain screening mammogram (Breast imaging reporting and data system [BI-RADS] = 0), and time to diagnostic resolution varies after BI-RADS = 0 screening mammogram. There is little data about factors associated with diagnostic resolution in patients of Chinese origin ("Chinese") receiving care in the US.
METHODS
We performed a retrospective analysis to identify patterns of diagnostic resolution in an urban US hospital with a large population of Chinese patients. We evaluated whether location of primary care provider (PCP) impacted time to resolution among Chinese patients, hypothesizing that patients with a PCP outside of the hospital would have longer time to diagnostic resolution than those patients with a PCP within the institution.
RESULTS
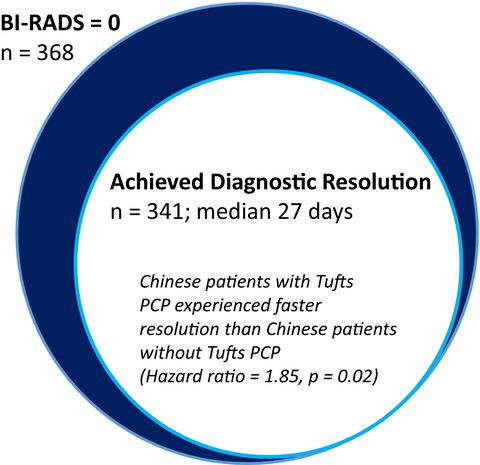
Between 2015 and 2016, 368 patients at Tufts Medical Center (Tufts MC) had resulting BI-RADS = 0 after screening mammogram. The majority of patients (341/368, 93%) achieved diagnostic resolution with median time to resolution 27 days (Q1: 14, Q3: 40). Seven percent (27/368) never achieved resolution. Among those with diagnostic resolution, 10% of patients required >60 days to achieve resolution. Chinese origin, no previous breast cancer, subsidized insurance, and outside referring physician were associated with longer time to resolution in univariable analysis. In multivariable regression, after adjusting for age, insurance, marital status, and prior breast cancer, Chinese patients with Tufts MC PCP experienced timelier diagnostic resolution vs Chinese patients without a Tufts MC PCP (hazard ratio [HR] = 1.85, P = .02). Location of PCP did not impact time to resolution among non-Chinese patients.
CONCLUSION
We identified patterns of diagnostic resolution in an urban hospital with a large historically underserved population. We found that Chinese patients without integrated primary care within the institution are at risk for delayed diagnostic resolution. Future interventions need to target at-risk patients to prevent loss of follow-up after uncertain screening mammogram.
更新日期:2020-03-11


























 京公网安备 11010802027423号
京公网安备 11010802027423号