Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Mortality and Hospitalizations for Dually Enrolled and Nondually Enrolled Medicare Beneficiaries Aged 65 Years or Older, 2004 to 2017
JAMA ( IF 120.7 ) Pub Date : 2020-03-10 , DOI: 10.1001/jama.2020.1021 Rishi K Wadhera 1 , Yun Wang 1, 2 , Jose F Figueroa 3, 4 , Francesca Dominici 2 , Robert W Yeh 1 , Karen E Joynt Maddox 5
JAMA ( IF 120.7 ) Pub Date : 2020-03-10 , DOI: 10.1001/jama.2020.1021 Rishi K Wadhera 1 , Yun Wang 1, 2 , Jose F Figueroa 3, 4 , Francesca Dominici 2 , Robert W Yeh 1 , Karen E Joynt Maddox 5
Affiliation
|
Importance
Medicare beneficiaries who are also enrolled in Medicaid (dually enrolled beneficiaries) have drawn the attention of policy makers because they comprise the poorest subset of the Medicare population; however, it is unclear how their outcomes have changed over time compared with those only enrolled in Medicare (nondually enrolled beneficiaries). Objective
To evaluate annual changes in all-cause mortality, hospitalization rates, and hospitalization-related mortality among dually enrolled beneficiaries and nondually enrolled beneficiaries. Design, Setting, and Participants
Serial cross-sectional study of Medicare fee-for-service beneficiaries aged 65 years or older between January 2004 and December 2017. The final date of follow-up was September 30, 2018. Exposures
Dual vs nondual enrollment status. Main Outcomes and Measures
Annual all-cause mortality rates; all-cause hospitalization rates; and in-hospital, 30-day, 1-year hospitalization-related mortality rates. Results
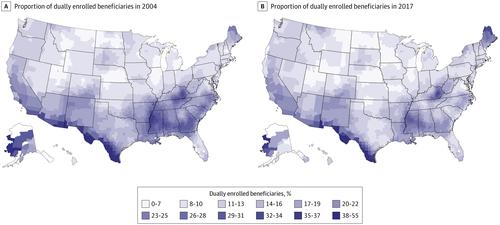
There were 71 017 608 unique Medicare beneficiaries aged 65 years or older (mean age, 75.6 [SD, 9.2] years; 54.9% female) enrolled in Medicare for at least 1 month from 2004 through 2017. Of these beneficiaries, 11 697 900 (16.5%) were dually enrolled in Medicare and Medicaid for at least 1 month. After adjusting for age, sex, and race, annual all-cause mortality rates declined from 8.5% (95% CI, 8.45%-8.56%) in 2004 to 8.1% (95% CI, 8.05%-8.13%) in 2017 among dually enrolled beneficiaries and from 4.1% (95% CI, 4.08%-4.13%) in 2004 to 3.8% (95% CI, 3.76%-3.79%) in 2017 among nondually enrolled beneficiaries. The difference in annual all-cause mortality between dually and nondually enrolled beneficiaries increased between 2004 (adjusted odds ratio, 2.09 [95% CI, 2.08-2.10]) and 2017 (adjusted odds ratio, 2.22 [95% CI, 2.21-2.23]) (P < .001 for interaction between dual enrollment status and time). All-cause hospitalizations per 100 000 beneficiary-years declined from 49 888 in 2004 to 41 121 in 2017 among dually enrolled beneficiaries (P < .001) and from 29 000 in 2004 to 22 601 in 2017 among nondually enrolled beneficiaries (P < .001); however, the difference between these groups widened between 2004 (adjusted risk ratio, 1.72 [95% CI, 1.71-1.73]) and 2017 (adjusted risk ratio, 1.83 [95% CI, 1.82-1.83]) (P < .001 for interaction). Among hospitalized beneficiaries, the risk-adjusted 30-day mortality rates declined from 10.3% (95% CI, 10.22%-10.33%) in 2004 to 10.1% (95% CI, 10.02%-10.20%) in 2017 among dually enrolled beneficiaries and from 8.5% (95% CI, 8.50%-8.56%) in 2004 to 8.1% (95% CI, 8.06%-8.13%) in 2017 among nondually enrolled beneficiaries. In contrast, 1-year mortality increased among hospitalized beneficiaries from 23.1% (95% CI, 23.05%-23.20%) in 2004 to 26.7% (95% CI, 26.58%-26.84%) in 2017 among dually enrolled beneficiaries and from 18.1% (95% CI, 18.11%-18.17%) in 2004 to 20.3% (95% CI, 20.21%-20.31%) in 2017 among nondually enrolled beneficiaries. The difference in hospitalization-related outcomes between dually and nondually enrolled beneficiaries persisted during the study period. Conclusions and Relevance
Among Medicare fee-for-service beneficiaries aged 65 years or older, dually enrolled beneficiaries had higher annual all-cause mortality, all-cause hospitalizations, and hospitalization-related mortality compared with nondually enrolled beneficiaries. Between 2004 and 2017, these differences did not decrease.
中文翻译:

2004 年至 2017 年 65 岁或以上双重登记和非双重登记医疗保险受益人的死亡率和住院率
重要的同时参加 Medicaid 的 Medicare 受益人(双重登记的受益人)已经引起了决策者的注意,因为他们是 Medicare 人口中最贫困的一部分;然而,与仅参加 Medicare 的人(非双重登记的受益人)相比,他们的结果如何随时间变化尚不清楚。目的 评估双重登记受益人和非双重登记受益人的全因死亡率、住院率和住院相关死亡率的年度变化。设计、设置和参与者 2004 年 1 月至 2017 年 12 月期间 65 岁或以上的医疗保险按服务收费受益人的连续横断面研究。随访的最终日期为 2018 年 9 月 30 日。暴露双重与非双重参保状态. 主要结果和措施 年全因死亡率;全因住院率;和住院 30 天、1 年住院相关死亡率。结果 从 2004 年到 2017 年,共有 71 017 608 名年龄在 65 岁或以上的独特医疗保险受益人(平均年龄为 75.6 [SD,9.2] 岁;54.9% 为女性)参加医疗保险至少 1 个月。在这些受益人中,有 11 697 90 (16.5%) 同时参加了医疗保险和医疗补助至少 1 个月。调整年龄、性别和种族后,年全因死亡率从 2004 年的 8.5%(95% CI,8.45%-8.56%)下降到 2017 年的 8.1%(95% CI,8.05%-8.13%),其中双重登记的受益人,非双重登记的受益人从 2004 年的 4.1%(95% CI,4.08%-4.13%)到 2017 年的 3.8%(95% CI,3.76%-3.79%)。在 2004 年(调整后的优势比,2.09 [95% CI,2.08-2.10])和 2017 年(调整后的优势比,2.22 [95% CI,2.21-2.23])之间,双重登记和非双重登记受益人的年全因死亡率差异有所增加)(对于双重注册状态和时间之间的交互,P < .001)。在双重登记受益人中,每 10 万受益人年的全因住院人数从 2004 年的 49 888 人下降到 2017 年的 41 121 人(P < .001),并从 2004 年的 29 000 人下降到非受益人中的 22 617 人(非受益人中的 22 601 人)。 001); 然而,这些组之间的差异在 2004 年(调整后风险比,1.72 [95% CI,1.71-1.73])和 2017 年(调整后风险比,1.83 [95% CI,1.82-1.83])之间扩大(P < .001相互作用)。在住院受益人中,风险调整后的 30 天死亡率从 10.3%(95% CI,10. 2004 年的 22%-10.33%) 到 2017 年的 10.1% (95% CI, 10.02%-10.20%) 在双重登记的受益人中和 2004 年的 8.5% (95% CI, 8.50%-8.56%) (9. % CI, 8.06%-8.13%) 在 2017 年在非双重登记的受益人中。相比之下,住院受益人的 1 年死亡率从 2004 年的 23.1%(95% CI,23.05%-23.20%)增加到 2017 年的 26.7%(95% CI,26.58%-26.84%)。在非双重登记的受益人中,2004 年的 %(95% CI,18.11%-18.17%)到 2017 年的 20.3%(95% CI,20.21%-20.31%)。在研究期间,双重登记和非双重登记受益人之间住院相关结果的差异持续存在。结论和相关性 在 65 岁或以上的 Medicare 按服务收费受益人中,双重登记受益人的年全因死亡率较高,与非双重登记受益人相比,全因住院和住院相关死亡率。从 2004 年到 2017 年,这些差异并没有减少。
更新日期:2020-03-10
中文翻译:

2004 年至 2017 年 65 岁或以上双重登记和非双重登记医疗保险受益人的死亡率和住院率
重要的同时参加 Medicaid 的 Medicare 受益人(双重登记的受益人)已经引起了决策者的注意,因为他们是 Medicare 人口中最贫困的一部分;然而,与仅参加 Medicare 的人(非双重登记的受益人)相比,他们的结果如何随时间变化尚不清楚。目的 评估双重登记受益人和非双重登记受益人的全因死亡率、住院率和住院相关死亡率的年度变化。设计、设置和参与者 2004 年 1 月至 2017 年 12 月期间 65 岁或以上的医疗保险按服务收费受益人的连续横断面研究。随访的最终日期为 2018 年 9 月 30 日。暴露双重与非双重参保状态. 主要结果和措施 年全因死亡率;全因住院率;和住院 30 天、1 年住院相关死亡率。结果 从 2004 年到 2017 年,共有 71 017 608 名年龄在 65 岁或以上的独特医疗保险受益人(平均年龄为 75.6 [SD,9.2] 岁;54.9% 为女性)参加医疗保险至少 1 个月。在这些受益人中,有 11 697 90 (16.5%) 同时参加了医疗保险和医疗补助至少 1 个月。调整年龄、性别和种族后,年全因死亡率从 2004 年的 8.5%(95% CI,8.45%-8.56%)下降到 2017 年的 8.1%(95% CI,8.05%-8.13%),其中双重登记的受益人,非双重登记的受益人从 2004 年的 4.1%(95% CI,4.08%-4.13%)到 2017 年的 3.8%(95% CI,3.76%-3.79%)。在 2004 年(调整后的优势比,2.09 [95% CI,2.08-2.10])和 2017 年(调整后的优势比,2.22 [95% CI,2.21-2.23])之间,双重登记和非双重登记受益人的年全因死亡率差异有所增加)(对于双重注册状态和时间之间的交互,P < .001)。在双重登记受益人中,每 10 万受益人年的全因住院人数从 2004 年的 49 888 人下降到 2017 年的 41 121 人(P < .001),并从 2004 年的 29 000 人下降到非受益人中的 22 617 人(非受益人中的 22 601 人)。 001); 然而,这些组之间的差异在 2004 年(调整后风险比,1.72 [95% CI,1.71-1.73])和 2017 年(调整后风险比,1.83 [95% CI,1.82-1.83])之间扩大(P < .001相互作用)。在住院受益人中,风险调整后的 30 天死亡率从 10.3%(95% CI,10. 2004 年的 22%-10.33%) 到 2017 年的 10.1% (95% CI, 10.02%-10.20%) 在双重登记的受益人中和 2004 年的 8.5% (95% CI, 8.50%-8.56%) (9. % CI, 8.06%-8.13%) 在 2017 年在非双重登记的受益人中。相比之下,住院受益人的 1 年死亡率从 2004 年的 23.1%(95% CI,23.05%-23.20%)增加到 2017 年的 26.7%(95% CI,26.58%-26.84%)。在非双重登记的受益人中,2004 年的 %(95% CI,18.11%-18.17%)到 2017 年的 20.3%(95% CI,20.21%-20.31%)。在研究期间,双重登记和非双重登记受益人之间住院相关结果的差异持续存在。结论和相关性 在 65 岁或以上的 Medicare 按服务收费受益人中,双重登记受益人的年全因死亡率较高,与非双重登记受益人相比,全因住院和住院相关死亡率。从 2004 年到 2017 年,这些差异并没有减少。


























 京公网安备 11010802027423号
京公网安备 11010802027423号