The Lancet Diabetes & Endocrinology ( IF 44.5 ) Pub Date : 2020-03-02 , DOI: 10.1016/s2213-8587(20)30024-3 Mengying Li 1 , Stefanie N Hinkle 1 , Katherine L Grantz 1 , Sungduk Kim 2 , Jagteshwar Grewal 1 , William A Grobman 3 , Daniel W Skupski 4 , Roger B Newman 5 , Edward K Chien 6 , Anthony Sciscione 7 , Noelia Zork 8 , Deborah A Wing 9 , Michael Nageotte 10 , Fasil Tekola-Ayele 1 , Germaine M Buck Louis 11 , Paul S Albert 2 , Cuilin Zhang 1
|
Background
The timepoint at which fetal growth begins to differ by maternal glycaemic status is not well understood. To address this lack of data, we examined gestational diabetes, impaired glucose tolerance, and early pregnancy glucose concentrations in relation to fetal growth trajectories.
Methods
This cohort study included 2458 pregnant women from the NICHD Fetal Growth Studies-Singletons study, which took place between 2009 and 2013. Women were recruited from 12 clinical centres in the USA. Women aged 18–40 years without major chronic conditions when entering pregnancy were included and those with records of neither glucose screening test or glucose tolerance test were excluded from the study. Women were enrolled at gestational weeks 8–13 and randomly assigned to four ultrasonogram schedules (Group A; weeks 16, 24, 30, 34; Group B: weeks 18, 26, 31, 35, 39; Group C: weeks 20, 28, 32, 36; Group D: weeks 22, 29, 33, 37, 41) to capture weekly fetal growth. Gestational diabetes, impaired glucose tolerance, and normal glucose tolerance were defined by medical record review. Glucose was measured in a subsample of women at weeks 10–14. We modelled fetal growth trajectories using linear mixed models with cubic splines. This study is registered with ClinicalTrials.gov, NCT00912132.
Findings
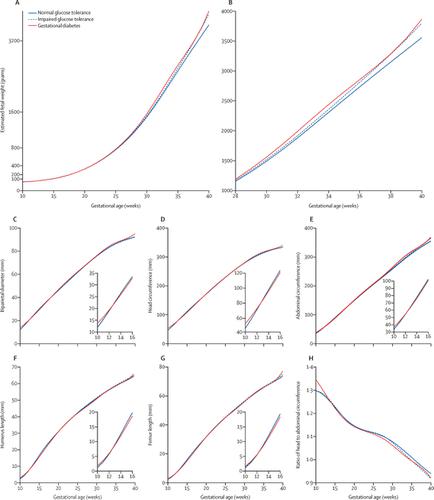
Of the 2458 women included in this study, 107 (4·4%) had gestational diabetes, 118 (4·8%) had impaired glucose tolerance, and 2020 (82·2%) had NGT. 213 women were excluded from the main analysis. The cohort with gestational diabetes was associated with a larger estimated fetal weight that started at week 20 and was significant at week 28–40 (at week 37: 3061 g [95% CI 2967–3164] for women with gestational diabetes vs 2943 g [2924–2962] for women with normal glucose tolerance, adjusted p=0·02). In addition, glucose levels at weeks 10–14 were positively associated with estimated fetal weight starting at week 23 and the association became significant at week 27 (at week 37: 3073 g [2983–3167] in the highest tertile vs 2853 g [2755–2955] in the lowest tertile, adjusted p=0·0009.
Interpretation
Gestational diabetes was associated with a larger fetal size that started at week 20 and became significant at gestational week 28. Efforts to mitigate gestational diabetes-related fetal overgrowth should start before 24–28 gestational weeks, when gestational diabetes is typically screened for in the USA.
Funding
National Institutes of Health.
中文翻译:

美国多种族人群妊娠期间的血糖状况和胎儿生长的纵向测量:一项前瞻性队列研究。
背景
胎儿生长状况因母体血糖状况而开始不同的时间点尚不清楚。为了解决这一数据不足的问题,我们检查了妊娠糖尿病,葡萄糖耐量降低和与胎儿生长轨迹相关的妊娠早期葡萄糖浓度。
方法
这项队列研究包括2009年至2013年间从NICHD胎儿生长研究-单项研究中选出的2458名孕妇。这些妇女是从美国12个临床中心招募的。纳入了18-40岁年龄段的妇女,这些妇女在进入怀孕时没有严重的慢性疾病,并且没有葡萄糖筛查测试或葡萄糖耐量测试记录的妇女也被排除在研究之外。妇女在妊娠第8-13周入组,随机分配给四个超声检查时间表(A组; 16、24、30、34周; B组:18、26、31、35、39周; C组:20、28周,32、36; D组:第22、29、33、37、41周,以捕获每周的胎儿生长情况。病史回顾定义了妊娠期糖尿病,糖耐量减低和葡萄糖耐量正常。在第10-14周的女性子样本中测量了葡萄糖。我们使用带有三次样条的线性混合模型对胎儿的生长轨迹进行建模。该研究已在ClinicalTrials.gov注册,NCT00912132。
发现
在这项研究中的2458名妇女中,有107名(4·4%)患有妊娠糖尿病,有118名(4·8%)的葡萄糖耐量受损,到2020年(82·2%)患有NGT。主要分析排除了213名妇女。妊娠糖尿病队列与较大的估计胎儿体重有关,该体重始于第20周,在第28-40周时显着(在妊娠糖尿病妇女中,第37周:3061 g [95%CI 2967-3164] vs 2943 g [ [2924–2962]对于葡萄糖耐量正常的女性,调整后的p = 0·02)。此外,从第23周开始,第10–14周的血糖水平与估计的胎儿体重呈正相关,而在第27周时,该关联变得显着(第37周:最高三分位数为3073 g [2983–3167],而2853 g [2755] –2955]在最低的三分位数中,调整p = 0·0009。
解释
妊娠糖尿病与较大的胎儿大小相关,该大小从20周开始,在妊娠第28周时变得明显。减轻妊娠糖尿病相关胎儿过度生长的工作应在妊娠24-28周之前开始,而在美国通常要筛查妊娠糖尿病。 。
资金
国立卫生研究院。


























 京公网安备 11010802027423号
京公网安备 11010802027423号