当前位置:
X-MOL 学术
›
Kidney Int.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
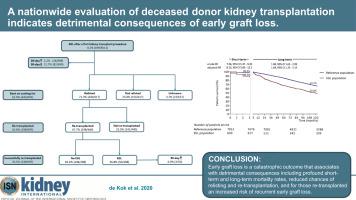
A nationwide evaluation of deceased donor kidney transplantation indicates detrimental consequences of early graft loss.
Kidney International ( IF 19.6 ) Pub Date : 2020-02-29 , DOI: 10.1016/j.kint.2020.01.043 Michèle J de Kok 1 , Alexander F Schaapherder 1 , Jacobus W Mensink 2 , Aiko P de Vries 3 , Marlies E Reinders 3 , Cynthia Konijn 4 , Frederike J Bemelman 5 , Jacqueline van de Wetering 6 , Arjan D van Zuilen 7 , Maarten H Christiaans 8 , Marije C Baas 9 , Azam S Nurmohamed 10 , Stefan P Berger 11 , Rutger J Ploeg 12 , Ian P Alwayn 1 , Jan H Lindeman 1
Kidney International ( IF 19.6 ) Pub Date : 2020-02-29 , DOI: 10.1016/j.kint.2020.01.043 Michèle J de Kok 1 , Alexander F Schaapherder 1 , Jacobus W Mensink 2 , Aiko P de Vries 3 , Marlies E Reinders 3 , Cynthia Konijn 4 , Frederike J Bemelman 5 , Jacqueline van de Wetering 6 , Arjan D van Zuilen 7 , Maarten H Christiaans 8 , Marije C Baas 9 , Azam S Nurmohamed 10 , Stefan P Berger 11 , Rutger J Ploeg 12 , Ian P Alwayn 1 , Jan H Lindeman 1
Affiliation
|
Early graft loss (EGL) is a feared outcome of kidney transplantation. Consequently, kidneys with an anticipated risk of EGL are declined for transplantation. In the most favorable scenario, with optimal use of available donor kidneys, the donor pool size is balanced by the risk of EGL, with a tradeoff dictated by the consequences of EGL. To gauge the consequence of EGL we systematically evaluated its impact in an observational study that included all 10,307 deceased-donor kidney transplantations performed in The Netherlands between 1990 and 2018. Incidence of EGL, defined as graft loss within 90 days, in primary transplantation was 8.2% (699/8,511). The main causes were graft rejection (30%), primary nonfunction (25%), and thrombosis or infarction (20%). EGL profoundly impacted short- and long-term patient survival (adjusted hazard ratio; 95% confidence interval: 8.2; 5.1-13.2 and 1.7; 1.3-2.1, respectively). Of the EGL recipients who survived 90 days after transplantation (617/699) only 440 of the 617 were relisted for re-transplantation. Of those relisted, only 298 were ultimately re-transplanted leading to an actual re-transplantation rate of 43%. Noticeably, re-transplantation was associated with a doubled incidence of EGL, but similar long-term graft survival (adjusted hazard ratio 1.1; 0.6-1.8). Thus, EGL after kidney transplantation is a medical catastrophe with high mortality rates, low relisting rates, and increased risk of recurrent EGL following re-transplantation. This implies that detrimental outcomes also involve convergence of risk factors in recipients with EGL. The 8.2% incidence of EGL minimally impacted population mortality, indicating this incidence is acceptable.
中文翻译:

全国范围内对已死的供体肾脏移植的评估表明,早期移植物丢失的有害后果。
早期移植物丢失(EGL)是肾脏移植的令人担忧的结果。因此,预期有EGL风险的肾脏将被移植。在最有利的情况下,最佳地利用可用的供体肾脏,供体库的大小将由EGL的风险平衡,而权衡取舍于EGL的后果。为了评估EGL的后果,我们在一项观察性研究中系统地评估了EGL的影响,该研究包括1990年至2018年在荷兰进行的所有10,307例死者肾移植。EGL的发生率是指初次移植90天之内的移植物损失为8.2 %(699 / 8,511)。主要原因是移植排斥反应(30%),原发性无功能(25%)和血栓形成或梗塞(20%)。EGL深刻影响了患者的短期和长期存活率(调整后的危险比;95%置信区间:8.2;5.1-13.2和1.7;1.3-2.1)。在移植后90天存活的EGL接受者(617/699)中,只有617人中的440人被重新上市。在重新列入名单的人中,最终只有298人被重新移植,导致实际再移植率为43%。值得注意的是,再移植与EGL的发生率增加了一倍,但移植物的长期存活率相似(风险比调整为1.1; 0.6-1.8)。因此,肾移植后的EGL是一种医学灾难,死亡率高,重新登记率低,并且在重新移植后复发EGL的风险增加。这意味着有害的结果还涉及EGL接受者的危险因素趋同。EGL的发生率8.2%对人口死亡率的影响最小,
更新日期:2020-02-29
中文翻译:

全国范围内对已死的供体肾脏移植的评估表明,早期移植物丢失的有害后果。
早期移植物丢失(EGL)是肾脏移植的令人担忧的结果。因此,预期有EGL风险的肾脏将被移植。在最有利的情况下,最佳地利用可用的供体肾脏,供体库的大小将由EGL的风险平衡,而权衡取舍于EGL的后果。为了评估EGL的后果,我们在一项观察性研究中系统地评估了EGL的影响,该研究包括1990年至2018年在荷兰进行的所有10,307例死者肾移植。EGL的发生率是指初次移植90天之内的移植物损失为8.2 %(699 / 8,511)。主要原因是移植排斥反应(30%),原发性无功能(25%)和血栓形成或梗塞(20%)。EGL深刻影响了患者的短期和长期存活率(调整后的危险比;95%置信区间:8.2;5.1-13.2和1.7;1.3-2.1)。在移植后90天存活的EGL接受者(617/699)中,只有617人中的440人被重新上市。在重新列入名单的人中,最终只有298人被重新移植,导致实际再移植率为43%。值得注意的是,再移植与EGL的发生率增加了一倍,但移植物的长期存活率相似(风险比调整为1.1; 0.6-1.8)。因此,肾移植后的EGL是一种医学灾难,死亡率高,重新登记率低,并且在重新移植后复发EGL的风险增加。这意味着有害的结果还涉及EGL接受者的危险因素趋同。EGL的发生率8.2%对人口死亡率的影响最小,



























 京公网安备 11010802027423号
京公网安备 11010802027423号