Nature Metabolism ( IF 20.8 ) Pub Date : 2020-02-20 , DOI: 10.1038/s42255-020-0171-3 Stephan Sachs 1, 2, 3, 4 , Aimée Bastidas-Ponce 1, 4, 5, 6 , Sophie Tritschler 1, 4, 7, 8 , Mostafa Bakhti 1, 4, 5 , Anika Böttcher 1, 4, 5 , Miguel A Sánchez-Garrido 2 , Marta Tarquis-Medina 1, 4, 5, 6 , Maximilian Kleinert 2, 9 , Katrin Fischer 2, 3 , Sigrid Jall 2, 3 , Alexandra Harger 2 , Erik Bader 1 , Sara Roscioni 1 , Siegfried Ussar 4, 6, 10 , Annette Feuchtinger 11 , Burcak Yesildag 12 , Aparna Neelakandhan 12 , Christine B Jensen 13 , Marion Cornu 13 , Bin Yang 14 , Brian Finan 14 , Richard D DiMarchi 14, 15 , Matthias H Tschöp 2, 3, 4 , Fabian J Theis 7, 8, 16 , Susanna M Hofmann 1, 4, 17 , Timo D Müller 2, 4, 18 , Heiko Lickert 1, 4, 5, 6
|
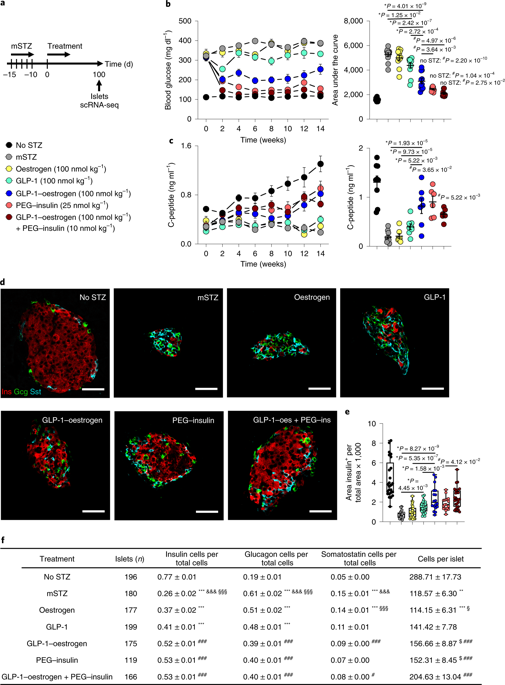
Dedifferentiation of insulin-secreting β cells in the islets of Langerhans has been proposed to be a major mechanism of β-cell dysfunction. Whether dedifferentiated β cells can be targeted by pharmacological intervention for diabetes remission, and ways in which this could be accomplished, are unknown as yet. Here we report the use of streptozotocin-induced diabetes to study β-cell dedifferentiation in mice. Single-cell RNA sequencing (scRNA-seq) of islets identified markers and pathways associated with β-cell dedifferentiation and dysfunction. Single and combinatorial pharmacology further show that insulin treatment triggers insulin receptor pathway activation in β cells and restores maturation and function for diabetes remission. Additional β-cell selective delivery of oestrogen by Glucagon-like peptide-1 (GLP-1–oestrogen conjugate) decreases daily insulin requirements by 60%, triggers oestrogen-specific activation of the endoplasmic-reticulum-associated protein degradation system, and further increases β-cell survival and regeneration. GLP-1–oestrogen also protects human β cells against cytokine-induced dysfunction. This study not only describes mechanisms of β-cell dedifferentiation and regeneration, but also reveals pharmacological entry points to target dedifferentiated β cells for diabetes remission.
中文翻译:

靶向药物治疗可恢复 β 细胞功能以缓解糖尿病。
已提出朗格汉斯胰岛中分泌胰岛素的 β 细胞去分化是 β 细胞功能障碍的主要机制。去分化的β细胞是否可以通过药物干预来缓解糖尿病,以及实现这一目标的方式,目前尚不清楚。在这里,我们报告了使用链脲佐菌素诱导的糖尿病来研究小鼠的 β 细胞去分化。胰岛的单细胞 RNA 测序 (scRNA-seq) 确定了与 β 细胞去分化和功能障碍相关的标志物和通路。单一和组合药理学进一步表明,胰岛素治疗触发 β 细胞中的胰岛素受体通路激活,并恢复糖尿病缓解的成熟和功能。胰高血糖素样肽 1(GLP-1-雌激素偶联物)额外的 β 细胞选择性递送雌激素可将每日胰岛素需求量降低 60%,触发内质网相关蛋白降解系统的雌激素特异性激活,并进一步增加β细胞的存活和再生。GLP-1-雌激素还保护人类 β 细胞免受细胞因子诱导的功能障碍。该研究不仅描述了 β 细胞去分化和再生的机制,还揭示了靶向去分化 β 细胞以缓解糖尿病的药理学切入点。GLP-1-雌激素还保护人类 β 细胞免受细胞因子诱导的功能障碍。该研究不仅描述了 β 细胞去分化和再生的机制,还揭示了靶向去分化 β 细胞以缓解糖尿病的药理学切入点。GLP-1-雌激素还保护人类 β 细胞免受细胞因子诱导的功能障碍。该研究不仅描述了 β 细胞去分化和再生的机制,还揭示了靶向去分化 β 细胞以缓解糖尿病的药理学切入点。

























 京公网安备 11010802027423号
京公网安备 11010802027423号