当前位置:
X-MOL 学术
›
Am. J. Kidney Dis.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
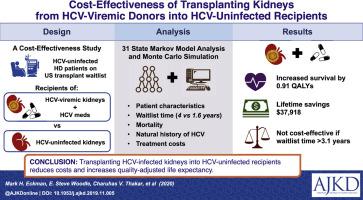
Cost-effectiveness of Using Kidneys From HCV-Viremic Donors for Transplantation Into HCV-Uninfected Recipients.
American Journal of Kidney Diseases ( IF 13.2 ) Pub Date : 2020-02-17 , DOI: 10.1053/j.ajkd.2019.11.005 Mark H Eckman 1 , E Steve Woodle 2 , Charuhas V Thakar 3 , Rita R Alloway 3 , Kenneth E Sherman 4
American Journal of Kidney Diseases ( IF 13.2 ) Pub Date : 2020-02-17 , DOI: 10.1053/j.ajkd.2019.11.005 Mark H Eckman 1 , E Steve Woodle 2 , Charuhas V Thakar 3 , Rita R Alloway 3 , Kenneth E Sherman 4
Affiliation
|
RATIONALE & OBJECTIVE
Less than 4% of patients with kidney failure receive kidney transplants. Although discard rates of hepatitis C virus (HCV)-viremic kidneys are declining, ~39% of HCV-viremic kidneys donated between 2018 and 2019 were discarded. Highly effective antiviral agents are now available to treat chronic HCV infection. Thus, our objective was to examine the cost-effectiveness of transplanting kidneys from HCV-viremic donors into HCV-uninfected recipients.
STUDY DESIGN
Markov state transition decision model. Data sources include Medline search results, bibliographies from relevant English language articles, Scientific Registry of Transplant Recipients, and the US Renal Data System.
SETTING & POPULATION
US patients receiving maintenance hemodialysis who are on kidney transplant waiting lists.
INTERVENTION(S)
Transplantation with an HCV-unexposed kidney versus transplantation with an HCV-viremic kidney and HCV treatment.
OUTCOMES
Effectiveness measured in quality-adjusted life-years and costs measured in 2018 US dollars.
MODEL, PERSPECTIVE, AND TIMEFRAME
We used a health care system perspective with a lifelong time horizon.
RESULTS
In the base-case analysis, transplantation with an HCV-viremic kidney was more effective and less costly than transplantation with an HCV-unexposed kidney because of the longer waiting times for HCV-unexposed kidneys, the substantial excess mortality risk while receiving dialysis, and the high efficacy of direct-acting antiviral agents for HCV infection. Transplantation with an HCV-viremic kidney was also preferred in sensitivity analyses of multiple model parameters. The strategy remained cost-effective unless waiting list time for an HCV-viremic kidney exceeded 3.1 years compared with the base-case value of 1.56 year.
LIMITATIONS
Estimates of waiting times for patients willing to accept an HCV-viremic kidney were based on data for patients who received HCV-viremic kidney transplants.
CONCLUSIONS
Transplanting kidneys from HCV-viremic donors into HCV-uninfected recipients increased quality-adjusted life expectancy and reduced costs compared with a strategy of transplanting kidneys from HCV-unexposed donors.
中文翻译:

使用来自HCV病毒捐赠者的肾脏移植到未感染HCV的接受者的成本效益。
理由和目标少于4%的肾衰竭患者接受肾脏移植。尽管丙型肝炎病毒(HCV)病毒性肾脏的丢弃率正在下降,但在2018年至2019年之间捐赠的HCV病毒性肾脏中约有39%被丢弃。现在可以使用高效抗病毒药来治疗慢性HCV感染。因此,我们的目标是检验从HCV病毒血症供体向未HCV感染的受者移植肾脏的成本效益。研究设计马尔可夫状态转移决策模型。数据来源包括Medline搜索结果,相关英语文章的参考书目,移植收件人的科学注册机构以及美国肾脏数据系统。地点和人口接受维持性血液透析的美国患者在肾脏移植等待名单上。干预措施:用未暴露HCV的肾脏进行移植与使用HCV病毒血症的肾脏进行移植以及HCV治疗。成果以质量调整生命年衡量的有效性和以2018年美元计量的成本。模型,透视图和时间框架我们使用了具有长期生命周期的医疗保健系统视角。结果在基本案例分析中,与HCV未暴露的肾脏相比,HCV病原性肾脏的移植更有效,成本更低,这是因为HCV未暴露的肾脏的等待时间更长,透析时存在相当大的死亡风险,以及直接作用抗病毒药对HCV感染的高疗效。在多个模型参数的敏感性分析中,还优选使用HCV-玻璃体肺移植。该策略仍然具有成本效益,除非等待HCV病毒血症的肾脏的等待时间超过3.1年,而基础病例值为1.56年。局限性愿意接受HCV病毒性肾移植的患者的等待时间估计是基于接受HCV病毒性肾移植的患者的数据。结论与从未暴露HCV的供体中移植肾脏的策略相比,将从HCV病毒血症的供体中移植肾脏到未感染HCV的接受者中,可以提高质量调整的预期寿命并降低成本。
更新日期:2020-02-17
中文翻译:

使用来自HCV病毒捐赠者的肾脏移植到未感染HCV的接受者的成本效益。
理由和目标少于4%的肾衰竭患者接受肾脏移植。尽管丙型肝炎病毒(HCV)病毒性肾脏的丢弃率正在下降,但在2018年至2019年之间捐赠的HCV病毒性肾脏中约有39%被丢弃。现在可以使用高效抗病毒药来治疗慢性HCV感染。因此,我们的目标是检验从HCV病毒血症供体向未HCV感染的受者移植肾脏的成本效益。研究设计马尔可夫状态转移决策模型。数据来源包括Medline搜索结果,相关英语文章的参考书目,移植收件人的科学注册机构以及美国肾脏数据系统。地点和人口接受维持性血液透析的美国患者在肾脏移植等待名单上。干预措施:用未暴露HCV的肾脏进行移植与使用HCV病毒血症的肾脏进行移植以及HCV治疗。成果以质量调整生命年衡量的有效性和以2018年美元计量的成本。模型,透视图和时间框架我们使用了具有长期生命周期的医疗保健系统视角。结果在基本案例分析中,与HCV未暴露的肾脏相比,HCV病原性肾脏的移植更有效,成本更低,这是因为HCV未暴露的肾脏的等待时间更长,透析时存在相当大的死亡风险,以及直接作用抗病毒药对HCV感染的高疗效。在多个模型参数的敏感性分析中,还优选使用HCV-玻璃体肺移植。该策略仍然具有成本效益,除非等待HCV病毒血症的肾脏的等待时间超过3.1年,而基础病例值为1.56年。局限性愿意接受HCV病毒性肾移植的患者的等待时间估计是基于接受HCV病毒性肾移植的患者的数据。结论与从未暴露HCV的供体中移植肾脏的策略相比,将从HCV病毒血症的供体中移植肾脏到未感染HCV的接受者中,可以提高质量调整的预期寿命并降低成本。



























 京公网安备 11010802027423号
京公网安备 11010802027423号