Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Electrical versus pharmacological cardioversion for emergency department patients with acute atrial fibrillation (RAFF2): a partial factorial randomised trial.
The Lancet ( IF 168.9 ) Pub Date : 2020-02-01 , DOI: 10.1016/s0140-6736(19)32994-0 Ian G Stiell 1 , Marco L A Sivilotti 2 , Monica Taljaard 3 , David Birnie 4 , Alain Vadeboncoeur 5 , Corinne M Hohl 6 , Andrew D McRae 7 , Brian H Rowe 8 , Robert J Brison 2 , Venkatesh Thiruganasambandamoorthy 1 , Laurent Macle 5 , Bjug Borgundvaag 9 , Judy Morris 10 , Eric Mercier 11 , Catherine M Clement 3 , Jennifer Brinkhurst 3 , Connor Sheehan 3 , Erica Brown 3 , Marie-Joe Nemnom 3 , George A Wells 12 , Jeffrey J Perry 1
The Lancet ( IF 168.9 ) Pub Date : 2020-02-01 , DOI: 10.1016/s0140-6736(19)32994-0 Ian G Stiell 1 , Marco L A Sivilotti 2 , Monica Taljaard 3 , David Birnie 4 , Alain Vadeboncoeur 5 , Corinne M Hohl 6 , Andrew D McRae 7 , Brian H Rowe 8 , Robert J Brison 2 , Venkatesh Thiruganasambandamoorthy 1 , Laurent Macle 5 , Bjug Borgundvaag 9 , Judy Morris 10 , Eric Mercier 11 , Catherine M Clement 3 , Jennifer Brinkhurst 3 , Connor Sheehan 3 , Erica Brown 3 , Marie-Joe Nemnom 3 , George A Wells 12 , Jeffrey J Perry 1
Affiliation
|
BACKGROUND
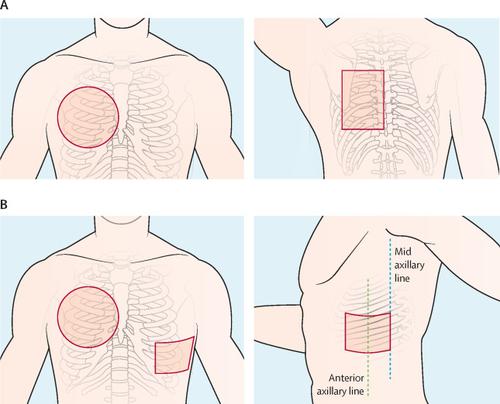
Acute atrial fibrillation is the most common arrythmia treated in the emergency department. Our primary aim was to compare conversion to sinus rhythm between pharmacological cardioversion followed by electrical cardioversion (drug-shock), and electrical cardioversion alone (shock-only). Our secondary aim was to compare the effectiveness of two pad positions for electrical cardioversion.
METHODS
We did a partial factorial trial of two protocols for patients with acute atrial fibrillation at 11 academic hospital emergency departments in Canada. We enrolled adult patients with acute atrial fibrillation. Protocol 1 was a randomised, blinded, placebo-controlled comparison of attempted pharmacological cardioversion with intravenous procainamide (15 mg/kg over 30 min) followed by electrical cardioversion if necessary (up to three shocks, each of ≥200 J), and placebo infusion followed by electrical cardioversion. For patients having electrical cardioversion, we used Protocol 2, a randomised, open-label, nested comparison of anteroposterior versus anterolateral pad positions. Patients were randomly assigned (1:1, stratified by study site) for Protocol 1 by on-site research personnel using an online electronic data capture system. Randomisation for Protocol 2 occurred 30 min after drug infusion for patients who had not converted and was stratified by site and Protocol 1 allocation. Patients and all research and emergency department staff were masked to treatment allocation for Protocol 1. The primary outcome was conversion to normal sinus rhythm for at least 30 min at any time after randomisation and up to a point immediately after three shocks. Protocol 1 was analysed by intention to treat and Protocol 2 excluded patients who did not receive electrical cardioversion. This study is registered at ClinicalTrials.gov, number NCT01891058.
FINDINGS
Between July 18, 2013, and Oct 17, 2018, we enrolled 396 patients, and none were lost to follow-up. In the drug-shock group (n=204), conversion to sinus rhythm occurred in 196 (96%) patients and in the shock-only group (n=192), conversion occurred in 176 (92%) patients (absolute difference 4%; 95% CI 0-9; p=0·07). The proportion of patients discharged home was 97% (n=198) versus 95% (n=183; p=0·60). 106 (52%) patients in the drug-shock group converted after drug infusion only. No patients had serious adverse events in follow-up. The different pad positions in Protocol 2 (n=244), had similar conversions to sinus rhythm (119 [94%] of 127 in anterolateral group vs 108 [92%] of 117 in anteroposterior group; p=0·68).
INTERPRETATION
Both the drug-shock and shock-only strategies were highly effective, rapid, and safe in restoring sinus rhythm for patients in the emergency department with acute atrial fibrillation, avoiding the need for return to hospital. The drug infusion worked for about half of patients and avoided the resource intensive procedural sedation required for electrical cardioversion. We also found no significant difference between the anterolateral and anteroposterior pad positions for electrical cardioversion. Immediate rhythm control for patients in the emergency department with acute atrial fibrillation leads to excellent outcomes.
FUNDING
Heart and Stroke Foundation of Canada and the Canadian Institutes of Health Research.
中文翻译:

急诊室急性心房颤动(RAFF2)患者的电复律与药理复律:一项部分因子随机试验。
背景技术急性房颤是急诊科治疗的最常见的心律失常。我们的主要目的是比较药理性电复律和电电复律(药物冲击)与单独电电复律(仅电击)之间的窦性心律转换。我们的次要目的是比较两个垫块位置对电复律的有效性。方法我们在加拿大的11个学术医院急诊科对急性房颤患者进行了两种方案的部分析因试验。我们招募了成年急性房颤患者。方案1是随机,盲法,安慰剂对照的比较,其中尝试用静脉注射普鲁卡因胺(30分钟内15 mg / kg)进行电复律,然后在必要时进行电复律(最多3次电击,≥200 J),并先进行安慰剂输注,然后进行电复律。对于有心脏电复律的患者,我们使用了方案2,即前后,前后外侧垫位置的随机,开放标签,嵌套式比较。使用在线电子数据捕获系统,由现场研究人员将患者随机分配(按研究地点分层,按1:1分层),用于研究方案1。对于未转化的患者,方案2的随机分配发生在药物输注后30分钟,并按部位和方案1分配进行分层。患者和所有研究及急诊部门工作人员都被掩盖了方案1的治疗分配。主要结果是在随机分组后的任何时间至少30分钟内转换为正常的窦性心律,直至三次电击后立即恢复。方案1的治疗意向进行了分析,方案2排除了未接受电复律的患者。该研究已在ClinicalTrials.gov上注册,编号为NCT01891058。结果在2013年7月18日至2018年10月17日之间,我们招募了396名患者,但均无失访。在药物休克组(n = 204)中,有196名患者(96%)发生了窦性心律的转变;在仅电击组(n = 192)中,有176(92%)名患者发生了窦性心律的转变(绝对差4 %; 95%CI 0-9; p = 0·07)。出院回家的患者比例为97%(n = 198),而95%(n = 183; p = 0·60)。仅在输注药物后,药物休克组的106名患者(52%)发生了转化。随访中无患者发生严重不良事件。协议2中的不同填充位置(n = 244),窦性心律转换相似(前外侧组为127的119 [94%],后侧组为117的108 [92%]; p = 0·68)。解释对于急诊患有急性心房颤动的患者,药物冲击法和仅电击疗法在恢复窦性心律方面都是非常有效,快速和安全的,从而避免了需要返回医院的情况。药物注入对大约一半的患者有效,并且避免了电复律所需的资源密集的镇静剂。我们也没有发现电复律的前外侧垫和前后垫位置之间没有显着差异。急诊室急性心房颤动患者的即时心律控制可带来极好的效果。
更新日期:2020-01-31
中文翻译:

急诊室急性心房颤动(RAFF2)患者的电复律与药理复律:一项部分因子随机试验。
背景技术急性房颤是急诊科治疗的最常见的心律失常。我们的主要目的是比较药理性电复律和电电复律(药物冲击)与单独电电复律(仅电击)之间的窦性心律转换。我们的次要目的是比较两个垫块位置对电复律的有效性。方法我们在加拿大的11个学术医院急诊科对急性房颤患者进行了两种方案的部分析因试验。我们招募了成年急性房颤患者。方案1是随机,盲法,安慰剂对照的比较,其中尝试用静脉注射普鲁卡因胺(30分钟内15 mg / kg)进行电复律,然后在必要时进行电复律(最多3次电击,≥200 J),并先进行安慰剂输注,然后进行电复律。对于有心脏电复律的患者,我们使用了方案2,即前后,前后外侧垫位置的随机,开放标签,嵌套式比较。使用在线电子数据捕获系统,由现场研究人员将患者随机分配(按研究地点分层,按1:1分层),用于研究方案1。对于未转化的患者,方案2的随机分配发生在药物输注后30分钟,并按部位和方案1分配进行分层。患者和所有研究及急诊部门工作人员都被掩盖了方案1的治疗分配。主要结果是在随机分组后的任何时间至少30分钟内转换为正常的窦性心律,直至三次电击后立即恢复。方案1的治疗意向进行了分析,方案2排除了未接受电复律的患者。该研究已在ClinicalTrials.gov上注册,编号为NCT01891058。结果在2013年7月18日至2018年10月17日之间,我们招募了396名患者,但均无失访。在药物休克组(n = 204)中,有196名患者(96%)发生了窦性心律的转变;在仅电击组(n = 192)中,有176(92%)名患者发生了窦性心律的转变(绝对差4 %; 95%CI 0-9; p = 0·07)。出院回家的患者比例为97%(n = 198),而95%(n = 183; p = 0·60)。仅在输注药物后,药物休克组的106名患者(52%)发生了转化。随访中无患者发生严重不良事件。协议2中的不同填充位置(n = 244),窦性心律转换相似(前外侧组为127的119 [94%],后侧组为117的108 [92%]; p = 0·68)。解释对于急诊患有急性心房颤动的患者,药物冲击法和仅电击疗法在恢复窦性心律方面都是非常有效,快速和安全的,从而避免了需要返回医院的情况。药物注入对大约一半的患者有效,并且避免了电复律所需的资源密集的镇静剂。我们也没有发现电复律的前外侧垫和前后垫位置之间没有显着差异。急诊室急性心房颤动患者的即时心律控制可带来极好的效果。


























 京公网安备 11010802027423号
京公网安备 11010802027423号