Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Deep learning for prediction of colorectal cancer outcome: a discovery and validation study.
The Lancet ( IF 168.9 ) Pub Date : 2020-02-01 , DOI: 10.1016/s0140-6736(19)32998-8 Ole-Johan Skrede 1 , Sepp De Raedt 1 , Andreas Kleppe 1 , Tarjei S Hveem 2 , Knut Liestøl 1 , John Maddison 2 , Hanne A Askautrud 2 , Manohar Pradhan 2 , John Arne Nesheim 2 , Fritz Albregtsen 1 , Inger Nina Farstad 3 , Enric Domingo 4 , David N Church 5 , Arild Nesbakken 6 , Neil A Shepherd 7 , Ian Tomlinson 8 , Rachel Kerr 4 , Marco Novelli 9 , David J Kerr 10 , Håvard E Danielsen 11
The Lancet ( IF 168.9 ) Pub Date : 2020-02-01 , DOI: 10.1016/s0140-6736(19)32998-8 Ole-Johan Skrede 1 , Sepp De Raedt 1 , Andreas Kleppe 1 , Tarjei S Hveem 2 , Knut Liestøl 1 , John Maddison 2 , Hanne A Askautrud 2 , Manohar Pradhan 2 , John Arne Nesheim 2 , Fritz Albregtsen 1 , Inger Nina Farstad 3 , Enric Domingo 4 , David N Church 5 , Arild Nesbakken 6 , Neil A Shepherd 7 , Ian Tomlinson 8 , Rachel Kerr 4 , Marco Novelli 9 , David J Kerr 10 , Håvard E Danielsen 11
Affiliation
|
BACKGROUND
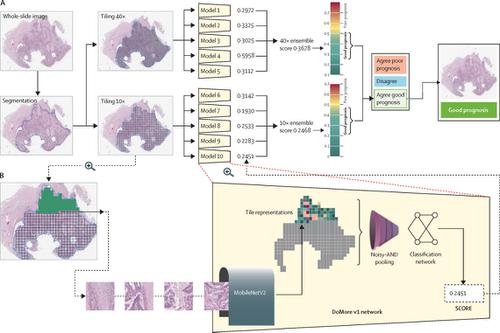
Improved markers of prognosis are needed to stratify patients with early-stage colorectal cancer to refine selection of adjuvant therapy. The aim of the present study was to develop a biomarker of patient outcome after primary colorectal cancer resection by directly analysing scanned conventional haematoxylin and eosin stained sections using deep learning.
METHODS
More than 12 000 000 image tiles from patients with a distinctly good or poor disease outcome from four cohorts were used to train a total of ten convolutional neural networks, purpose-built for classifying supersized heterogeneous images. A prognostic biomarker integrating the ten networks was determined using patients with a non-distinct outcome. The marker was tested on 920 patients with slides prepared in the UK, and then independently validated according to a predefined protocol in 1122 patients treated with single-agent capecitabine using slides prepared in Norway. All cohorts included only patients with resectable tumours, and a formalin-fixed, paraffin-embedded tumour tissue block available for analysis. The primary outcome was cancer-specific survival.
FINDINGS
828 patients from four cohorts had a distinct outcome and were used as a training cohort to obtain clear ground truth. 1645 patients had a non-distinct outcome and were used for tuning. The biomarker provided a hazard ratio for poor versus good prognosis of 3·84 (95% CI 2·72-5·43; p<0·0001) in the primary analysis of the validation cohort, and 3·04 (2·07-4·47; p<0·0001) after adjusting for established prognostic markers significant in univariable analyses of the same cohort, which were pN stage, pT stage, lymphatic invasion, and venous vascular invasion.
INTERPRETATION
A clinically useful prognostic marker was developed using deep learning allied to digital scanning of conventional haematoxylin and eosin stained tumour tissue sections. The assay has been extensively evaluated in large, independent patient populations, correlates with and outperforms established molecular and morphological prognostic markers, and gives consistent results across tumour and nodal stage. The biomarker stratified stage II and III patients into sufficiently distinct prognostic groups that potentially could be used to guide selection of adjuvant treatment by avoiding therapy in very low risk groups and identifying patients who would benefit from more intensive treatment regimes.
FUNDING
The Research Council of Norway.
中文翻译:

深度学习预测大肠癌预后:一项发现和验证研究。
背景技术需要改善的预后标志物以对早期结直肠癌患者进行分层以改善辅助疗法的选择。本研究的目的是通过使用深度学习直接分析扫描的常规苏木精和曙红染色切片来开发原发性结直肠癌切除术后患者预后的生物标志物。方法用来自四个队列的疾病结果明显好或差的患者提供的超过12000000张图像块用于训练总共十个卷积神经网络,这些卷积神经网络是专为对超大型异类图像进行分类而构建的。使用未明确结果的患者确定整合了十个网络的预后生物标志物。该标志物已在英国制备的920例载玻片上进行了测试,然后根据预先定义的方案对在挪威使用制备的载玻片单药卡培他滨治疗的1122名患者进行独立验证。所有队列仅包括可切除肿瘤的患者,以及可用于分析的福尔马林固定,石蜡包埋的肿瘤组织块。主要结果是特定于癌症的存活率。结果来自四个队列的828例患者有不同的预后,并被用作训练队列以获取明确的事实真相。1645例患者的结果无明显差异,用于调整。在验证队列的主要分析中,该生物标志物为不良与良好预后的危险比为3·84(95%CI 2·72-5·43; p <0·0001),而危险比为3·04(2·07 -4·47; p <0·0001)调整了在同一队列的单变量分析中显着的已建立的预后指标后,分别是pN期,pT期,淋巴管浸润和静脉血管浸润。解释使用与传统苏木精和曙红染色的肿瘤组织切片进行数字扫描相关的深度学习,开发了临床上有用的预后指标。该测定法已在众多独立患者群体中进行了广泛评估,其与既定的分子和形态学预后标记物相关并优于其,并在肿瘤和淋巴结分期提供了一致的结果。生物标志物将II期和III期患者分为足够不同的预后组,这些预后组可以通过避免在极低风险的人群中进行治疗并确定可从更深入的治疗方案中受益的患者来指导辅助治疗的选择。资金挪威研究委员会。淋巴管浸润和静脉血管浸润。解释使用与传统苏木精和曙红染色的肿瘤组织切片进行数字扫描相关的深度学习,开发了临床上有用的预后指标。该测定法已在众多独立患者群体中进行了广泛评估,其与既定的分子和形态学预后标记物相关并优于其,并在肿瘤和淋巴结分期提供了一致的结果。生物标志物将II期和III期患者分为足够不同的预后组,这些预后组可以通过避免在极低风险的人群中进行治疗并确定可从更深入的治疗方案中受益的患者来指导辅助治疗的选择。资金挪威研究委员会。淋巴管浸润和静脉血管浸润。解释使用与传统苏木精和曙红染色的肿瘤组织切片进行数字扫描相关的深度学习,开发了临床上有用的预后指标。该测定法已在众多独立患者群体中进行了广泛评估,其与既定的分子和形态学预后标记物相关并优于其,并在肿瘤和淋巴结分期提供了一致的结果。生物标志物将II期和III期患者分为足够不同的预后组,这些预后组可以通过避免在极低风险的人群中进行治疗并确定可从更深入的治疗方案中受益的患者来指导辅助治疗的选择。资金挪威研究委员会。解释使用与传统苏木精和曙红染色的肿瘤组织切片进行数字扫描相关的深度学习,开发了临床上有用的预后指标。该测定法已在众多独立患者群体中进行了广泛评估,其与既定的分子和形态学预后标记物相关并优于其,并在肿瘤和淋巴结分期提供了一致的结果。生物标志物将II期和III期患者分为足够不同的预后组,这些预后组可以通过避免在极低风险的人群中进行治疗并确定可从更深入的治疗方案中受益的患者来指导辅助治疗的选择。资金挪威研究委员会。解释使用与传统苏木精和曙红染色的肿瘤组织切片进行数字扫描相关的深度学习,开发了临床上有用的预后指标。该测定法已在众多独立患者群体中进行了广泛评估,其与既定的分子和形态学预后标记物相关并优于其,并在肿瘤和淋巴结分期提供了一致的结果。生物标志物将II期和III期患者分为足够不同的预后组,这些预后组可以通过避免在极低风险的人群中进行治疗并确定可从更深入的治疗方案中受益的患者来指导辅助治疗的选择。资金挪威研究委员会。
更新日期:2020-01-31
中文翻译:

深度学习预测大肠癌预后:一项发现和验证研究。
背景技术需要改善的预后标志物以对早期结直肠癌患者进行分层以改善辅助疗法的选择。本研究的目的是通过使用深度学习直接分析扫描的常规苏木精和曙红染色切片来开发原发性结直肠癌切除术后患者预后的生物标志物。方法用来自四个队列的疾病结果明显好或差的患者提供的超过12000000张图像块用于训练总共十个卷积神经网络,这些卷积神经网络是专为对超大型异类图像进行分类而构建的。使用未明确结果的患者确定整合了十个网络的预后生物标志物。该标志物已在英国制备的920例载玻片上进行了测试,然后根据预先定义的方案对在挪威使用制备的载玻片单药卡培他滨治疗的1122名患者进行独立验证。所有队列仅包括可切除肿瘤的患者,以及可用于分析的福尔马林固定,石蜡包埋的肿瘤组织块。主要结果是特定于癌症的存活率。结果来自四个队列的828例患者有不同的预后,并被用作训练队列以获取明确的事实真相。1645例患者的结果无明显差异,用于调整。在验证队列的主要分析中,该生物标志物为不良与良好预后的危险比为3·84(95%CI 2·72-5·43; p <0·0001),而危险比为3·04(2·07 -4·47; p <0·0001)调整了在同一队列的单变量分析中显着的已建立的预后指标后,分别是pN期,pT期,淋巴管浸润和静脉血管浸润。解释使用与传统苏木精和曙红染色的肿瘤组织切片进行数字扫描相关的深度学习,开发了临床上有用的预后指标。该测定法已在众多独立患者群体中进行了广泛评估,其与既定的分子和形态学预后标记物相关并优于其,并在肿瘤和淋巴结分期提供了一致的结果。生物标志物将II期和III期患者分为足够不同的预后组,这些预后组可以通过避免在极低风险的人群中进行治疗并确定可从更深入的治疗方案中受益的患者来指导辅助治疗的选择。资金挪威研究委员会。淋巴管浸润和静脉血管浸润。解释使用与传统苏木精和曙红染色的肿瘤组织切片进行数字扫描相关的深度学习,开发了临床上有用的预后指标。该测定法已在众多独立患者群体中进行了广泛评估,其与既定的分子和形态学预后标记物相关并优于其,并在肿瘤和淋巴结分期提供了一致的结果。生物标志物将II期和III期患者分为足够不同的预后组,这些预后组可以通过避免在极低风险的人群中进行治疗并确定可从更深入的治疗方案中受益的患者来指导辅助治疗的选择。资金挪威研究委员会。淋巴管浸润和静脉血管浸润。解释使用与传统苏木精和曙红染色的肿瘤组织切片进行数字扫描相关的深度学习,开发了临床上有用的预后指标。该测定法已在众多独立患者群体中进行了广泛评估,其与既定的分子和形态学预后标记物相关并优于其,并在肿瘤和淋巴结分期提供了一致的结果。生物标志物将II期和III期患者分为足够不同的预后组,这些预后组可以通过避免在极低风险的人群中进行治疗并确定可从更深入的治疗方案中受益的患者来指导辅助治疗的选择。资金挪威研究委员会。解释使用与传统苏木精和曙红染色的肿瘤组织切片进行数字扫描相关的深度学习,开发了临床上有用的预后指标。该测定法已在众多独立患者群体中进行了广泛评估,其与既定的分子和形态学预后标记物相关并优于其,并在肿瘤和淋巴结分期提供了一致的结果。生物标志物将II期和III期患者分为足够不同的预后组,这些预后组可以通过避免在极低风险的人群中进行治疗并确定可从更深入的治疗方案中受益的患者来指导辅助治疗的选择。资金挪威研究委员会。解释使用与传统苏木精和曙红染色的肿瘤组织切片进行数字扫描相关的深度学习,开发了临床上有用的预后指标。该测定法已在众多独立患者群体中进行了广泛评估,其与既定的分子和形态学预后标记物相关并优于其,并在肿瘤和淋巴结分期提供了一致的结果。生物标志物将II期和III期患者分为足够不同的预后组,这些预后组可以通过避免在极低风险的人群中进行治疗并确定可从更深入的治疗方案中受益的患者来指导辅助治疗的选择。资金挪威研究委员会。


























 京公网安备 11010802027423号
京公网安备 11010802027423号