Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Yield of a Public Health Screening of Children for Islet Autoantibodies in Bavaria, Germany
JAMA ( IF 120.7 ) Pub Date : 2020-01-28 , DOI: 10.1001/jama.2019.21565 Anette-Gabriele Ziegler 1, 2, 3 , Kerstin Kick 1, 3 , Ezio Bonifacio 4, 5, 6 , Florian Haupt 1, 3 , Markus Hippich 1, 3 , Desiree Dunstheimer 7 , Martin Lang 8 , Otto Laub 9 , Katharina Warncke 10 , Karin Lange 11 , Robin Assfalg 1, 3 , Manja Jolink 1, 3 , Christiane Winkler 1, 3 , Peter Achenbach 1, 2, 3 ,
JAMA ( IF 120.7 ) Pub Date : 2020-01-28 , DOI: 10.1001/jama.2019.21565 Anette-Gabriele Ziegler 1, 2, 3 , Kerstin Kick 1, 3 , Ezio Bonifacio 4, 5, 6 , Florian Haupt 1, 3 , Markus Hippich 1, 3 , Desiree Dunstheimer 7 , Martin Lang 8 , Otto Laub 9 , Katharina Warncke 10 , Karin Lange 11 , Robin Assfalg 1, 3 , Manja Jolink 1, 3 , Christiane Winkler 1, 3 , Peter Achenbach 1, 2, 3 ,
Affiliation
|
Importance
Public health screening for type 1 diabetes in its presymptomatic stages may reduce disease severity and burden on a population level. Objective
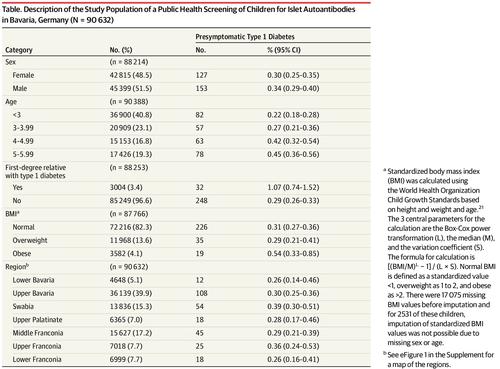
To determine the prevalence of presymptomatic type 1 diabetes in children participating in a public health screening program for islet autoantibodies and the risk for progression to clinical diabetes. Design, Setting, and Participants
Screening for islet autoantibodies was offered to children aged 1.75 to 5.99 years in Bavaria, Germany, between 2015 and 2019 by primary care pediatricians during well-baby visits. Families of children with multiple islet autoantibodies (presymptomatic type 1 diabetes) were invited to participate in a program of diabetes education, metabolic staging, assessment of psychological stress associated with diagnosis, and prospective follow-up for progression to clinical diabetes until July 31, 2019. Exposures
Measurement of islet autoantibodies. Main Outcomes and Measures
The primary outcome was presymptomatic type 1 diabetes, defined by 2 or more islet autoantibodies, with categorization into stages 1 (normoglycemia), 2 (dysglycemia), or 3 (clinical) type 1 diabetes. Secondary outcomes were the frequency of diabetic ketoacidosis and parental psychological stress, assessed by the Patient Health Questionnaire-9 (range, 0-27; higher scores indicate worse depression; ≤4 indicates no to minimal depression; >20 indicates severe depression). Results
Of 90 632 children screened (median [interquartile range {IQR}] age, 3.1 [2.1-4.2] years; 48.5% girls), 280 (0.31%; 95% CI, 0.27-0.35) had presymptomatic type 1 diabetes, including 196 (0.22%) with stage 1, 17 (0.02%) with stage 2, 26 (0.03%) with stage 3, and 41 who were not staged. After a median (IQR) follow-up of 2.4 (1.0-3.2) years, another 36 children developed stage 3 type 1 diabetes. The 3-year cumulative risk for stage 3 type 1 diabetes in the 280 children with presymptomatic type 1 diabetes was 24.9% ([95% CI, 18.5%-30.7%]; 54 cases; annualized rate, 9.0%). Two children had diabetic ketoacidosis. Median (IQR) psychological stress scores were significantly increased at the time of metabolic staging in mothers of children with presymptomatic type 1 diabetes (3 [1-7]) compared with mothers of children without islet autoantibodies (2 [1-4]) (P = .002), but declined after 12 months of follow-up (2 [0-4]) (P < .001). Conclusions and Relevance
Among children aged 2 to 5 years in Bavaria, Germany, a program of primary care-based screening showed an islet autoantibody prevalence of 0.31%. These findings may inform considerations of population-based screening of children for islet autoantibodies.
中文翻译:

德国巴伐利亚州儿童胰岛自身抗体的公共卫生筛查结果
重要性 在症状前阶段对 1 型糖尿病进行公共卫生筛查可能会降低疾病的严重程度和人群的负担。目的 确定参与胰岛自身抗体公共卫生筛查项目的儿童中症状前 1 型糖尿病的患病率以及进展为临床糖尿病的风险。2015 年至 2019 年期间,初级保健儿科医生在婴儿就诊期间为德国巴伐利亚州 1.75 至 5.99 岁的儿童提供了胰岛自身抗体的设计、设置和参与者筛查。邀请患有多种胰岛自身抗体(症状前 1 型糖尿病)儿童的家庭参加糖尿病教育、代谢分期、与诊断相关的心理压力评估、以及进展为临床糖尿病的前瞻性随访,直至 2019 年 7 月 31 日。胰岛自身抗体的暴露测量。主要结果和测量 主要结果是症状前 1 型糖尿病,定义为 2 种或更多胰岛自身抗体,分为 1 期(血糖正常)、2 期(血糖异常)或 3 期(临床)1 型糖尿病。次要结果是糖尿病酮症酸中毒和父母心理压力的频率,由患者健康问卷 9 评估(范围,0-27;得分越高表示抑郁症越严重;≤4 表示没有至轻微抑郁症;>20 表示严重抑郁症)。结果 在接受筛查的 90 632 名儿童中(中位数 [四分位距 {IQR}] 年龄,3.1 [2.1-4.2] 岁;48.5% 的女孩),280 名(0.31%;95% CI,0.27-0.35)患有症状前 1 型糖尿病,包括196 (0.22%) 阶段 1, 17 (0. 02%) 与第 2 阶段,26 (0.03%) 与第 3 阶段和 41 未上演。在 2.4 (1.0-3.2) 年的中位 (IQR) 随访后,另外 36 名儿童患上了 3 期 1 型糖尿病。在 280 名症状前 1 型糖尿病儿童中,3 年 3 期 1 型糖尿病的累积风险为 24.9%([95% CI,18.5%-30.7%];54 例;年化率为 9.0%)。两名儿童患有糖尿病酮症酸中毒。与没有胰岛自身抗体的儿童的母亲相比 (2 [1-4]),患有症状前 1 型糖尿病 (3 [1-7]) 的儿童的母亲在代谢分期时心理压力评分中位数 (IQR) 显着增加 (2 [1-4])。 P = .002),但在 12 个月的随访后下降 (2 [0-4]) (P < .001)。结论和相关性在德国巴伐利亚州 2 至 5 岁的儿童中,一项基于初级保健的筛查计划显示胰岛自身抗体的患病率为 0.31%。这些发现可能有助于考虑基于人群的儿童胰岛自身抗体筛查。
更新日期:2020-01-28
中文翻译:

德国巴伐利亚州儿童胰岛自身抗体的公共卫生筛查结果
重要性 在症状前阶段对 1 型糖尿病进行公共卫生筛查可能会降低疾病的严重程度和人群的负担。目的 确定参与胰岛自身抗体公共卫生筛查项目的儿童中症状前 1 型糖尿病的患病率以及进展为临床糖尿病的风险。2015 年至 2019 年期间,初级保健儿科医生在婴儿就诊期间为德国巴伐利亚州 1.75 至 5.99 岁的儿童提供了胰岛自身抗体的设计、设置和参与者筛查。邀请患有多种胰岛自身抗体(症状前 1 型糖尿病)儿童的家庭参加糖尿病教育、代谢分期、与诊断相关的心理压力评估、以及进展为临床糖尿病的前瞻性随访,直至 2019 年 7 月 31 日。胰岛自身抗体的暴露测量。主要结果和测量 主要结果是症状前 1 型糖尿病,定义为 2 种或更多胰岛自身抗体,分为 1 期(血糖正常)、2 期(血糖异常)或 3 期(临床)1 型糖尿病。次要结果是糖尿病酮症酸中毒和父母心理压力的频率,由患者健康问卷 9 评估(范围,0-27;得分越高表示抑郁症越严重;≤4 表示没有至轻微抑郁症;>20 表示严重抑郁症)。结果 在接受筛查的 90 632 名儿童中(中位数 [四分位距 {IQR}] 年龄,3.1 [2.1-4.2] 岁;48.5% 的女孩),280 名(0.31%;95% CI,0.27-0.35)患有症状前 1 型糖尿病,包括196 (0.22%) 阶段 1, 17 (0. 02%) 与第 2 阶段,26 (0.03%) 与第 3 阶段和 41 未上演。在 2.4 (1.0-3.2) 年的中位 (IQR) 随访后,另外 36 名儿童患上了 3 期 1 型糖尿病。在 280 名症状前 1 型糖尿病儿童中,3 年 3 期 1 型糖尿病的累积风险为 24.9%([95% CI,18.5%-30.7%];54 例;年化率为 9.0%)。两名儿童患有糖尿病酮症酸中毒。与没有胰岛自身抗体的儿童的母亲相比 (2 [1-4]),患有症状前 1 型糖尿病 (3 [1-7]) 的儿童的母亲在代谢分期时心理压力评分中位数 (IQR) 显着增加 (2 [1-4])。 P = .002),但在 12 个月的随访后下降 (2 [0-4]) (P < .001)。结论和相关性在德国巴伐利亚州 2 至 5 岁的儿童中,一项基于初级保健的筛查计划显示胰岛自身抗体的患病率为 0.31%。这些发现可能有助于考虑基于人群的儿童胰岛自身抗体筛查。



























 京公网安备 11010802027423号
京公网安备 11010802027423号