Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Peer distribution of HIV self-test kits to men who have sex with men to identify undiagnosed HIV infection in Uganda: A pilot study.
PLOS ONE ( IF 3.7 ) Pub Date : 2020-01-23 , DOI: 10.1371/journal.pone.0227741 Stephen Okoboi 1, 2 , Oucul Lazarus 3 , Barbara Castelnuovo 1 , Mastula Nanfuka 3 , Andrew Kambugu 1 , Andrew Mujugira 1, 4 , Rachel King 4, 5
PLOS ONE ( IF 3.7 ) Pub Date : 2020-01-23 , DOI: 10.1371/journal.pone.0227741 Stephen Okoboi 1, 2 , Oucul Lazarus 3 , Barbara Castelnuovo 1 , Mastula Nanfuka 3 , Andrew Kambugu 1 , Andrew Mujugira 1, 4 , Rachel King 4, 5
Affiliation
|
INTRODUCTION
One-in-three men who have sex with men (MSM) in Uganda have never tested for HIV. Peer-driven HIV testing strategies could increase testing coverage among non-testers. We evaluated the yield of peer distributed HIV self-test kits compared with standard-of-care testing approaches in identifying undiagnosed HIV infection.
METHODS
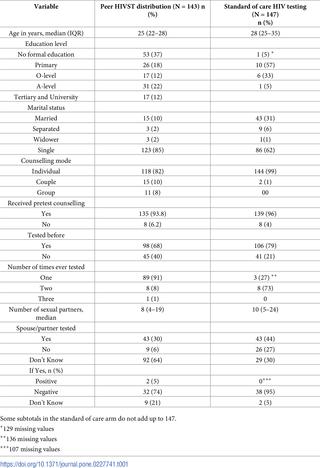
From June to August 2018, we conducted a pilot study of secondary distribution of HIV self-testing (HIVST) through MSM peer networks at The AIDS Support Organization (TASO) centres in Entebbe and Masaka. Peers were trained in HIVST use and basic HIV counselling. Each peer distributed 10 HIVST kits in one wave to MSM who had not tested in the previous six months. Participants who tested positive were linked by peers to HIV care. The primary outcome was the proportion of undiagnosed HIV infections. Data were analysed descriptively.
RESULTS
A total of 297 participants were included in the analysis, of whom 150 received HIVST (intervention). The median age of HIVST recipients was 25 years (interquartile range [IQR], 22-28) compared to 28 years IQR (25-35) for 147 MSM tested using standard-of-care (SOC) strategies. One hundred forty-three MSM (95%) completed HIVST, of which 32% had never tested for HIV. A total of 12 participants were newly diagnosed with HIV infection: 8 in the peer HIVST group and 4 in the SOC group [5.6% vs 2.7%, respectively; P = 0.02]. All participants newly diagnosed with HIV infection received confirmatory HIV testing and were initiated on antiretroviral therapy.
CONCLUSION
Peer distribution of HIVST through MSM networks is feasible and effective and could diagnose more new HIV infections than SOC approaches. Public health programs should consider scaling up peer-delivered HIVST for MSM.
中文翻译:

在乌干达向与男性发生性关系的男性同伴分发艾滋病毒自我检测试剂盒,以鉴定在乌干达未诊断出的艾滋病毒感染。
引言在乌干达,有三分之一的男男性接触者(MSM)从未接受过HIV检测。同行驱动的艾滋病毒检测策略可以增加非检测者的检测范围。在鉴定未诊断的HIV感染时,我们评估了同龄人分发的HIV自测工具包与标准护理测试方法相比的产量。方法从2018年6月至2018年8月,我们在恩德培和马萨卡的艾滋病支持组织(TASO)中心通过MSM对等网络进行了艾滋病毒自我测试(HIVST)的二次分发的初步研究。对同伴进行了HIVST使用和基本HIV咨询的培训。每位同伴一口气向MSM分发了10个HIVST试剂盒,而MSM在过去六个月中没有进行过测试。测试结果呈阳性的参与者通过同伴与艾滋病毒治疗联系在一起。主要结果是未确诊的艾滋病毒感染比例。对数据进行描述性分析。结果分析共纳入297位参与者,其中150位接受了HIVST(干预)。HIVST接受者的中位年龄为25岁(四分位间距[IQR],22-28岁),而采用照护标准(SOC)策略测试的147名MSM患者的中位年龄为28岁IQR(25-35岁)。一百四十三名男男性接触者(占95%)完成了HIVST,其中32%从未接受过HIV检测。共有12名新近被诊断出感染了HIV的参与者:同伴的HIVST组为8名,SOC组为4名[分别为5.6%和2.7%;P = 0.02]。所有新诊断出患有HIV感染的参与者都接受了确诊的HIV测试,并开始接受抗逆转录病毒疗法。结论通过MSM网络对HIVST进行对等分发是可行和有效的,并且比SOC方法可以诊断出更多的新HIV感染。
更新日期:2020-01-24
中文翻译:

在乌干达向与男性发生性关系的男性同伴分发艾滋病毒自我检测试剂盒,以鉴定在乌干达未诊断出的艾滋病毒感染。
引言在乌干达,有三分之一的男男性接触者(MSM)从未接受过HIV检测。同行驱动的艾滋病毒检测策略可以增加非检测者的检测范围。在鉴定未诊断的HIV感染时,我们评估了同龄人分发的HIV自测工具包与标准护理测试方法相比的产量。方法从2018年6月至2018年8月,我们在恩德培和马萨卡的艾滋病支持组织(TASO)中心通过MSM对等网络进行了艾滋病毒自我测试(HIVST)的二次分发的初步研究。对同伴进行了HIVST使用和基本HIV咨询的培训。每位同伴一口气向MSM分发了10个HIVST试剂盒,而MSM在过去六个月中没有进行过测试。测试结果呈阳性的参与者通过同伴与艾滋病毒治疗联系在一起。主要结果是未确诊的艾滋病毒感染比例。对数据进行描述性分析。结果分析共纳入297位参与者,其中150位接受了HIVST(干预)。HIVST接受者的中位年龄为25岁(四分位间距[IQR],22-28岁),而采用照护标准(SOC)策略测试的147名MSM患者的中位年龄为28岁IQR(25-35岁)。一百四十三名男男性接触者(占95%)完成了HIVST,其中32%从未接受过HIV检测。共有12名新近被诊断出感染了HIV的参与者:同伴的HIVST组为8名,SOC组为4名[分别为5.6%和2.7%;P = 0.02]。所有新诊断出患有HIV感染的参与者都接受了确诊的HIV测试,并开始接受抗逆转录病毒疗法。结论通过MSM网络对HIVST进行对等分发是可行和有效的,并且比SOC方法可以诊断出更多的新HIV感染。


























 京公网安备 11010802027423号
京公网安备 11010802027423号