The Lancet Global Health ( IF 34.3 ) Pub Date : 2020-01-22 , DOI: 10.1016/s2214-109x(19)30527-3 Louise Kuhn 1 , Rakiya Saidu 2 , Rosalind Boa 2 , Ana Tergas 3 , Jennifer Moodley 4 , David Persing 5 , Scott Campbell 5 , Wei-Yann Tsai 6 , Thomas C Wright 7 , Lynette Denny 2
|
Background
HPV-based screen and treat is the recommended approach for cervical cancer screening in low-resource settings, but quite low specificity of human papillomavirus (HPV) testing, particularly in women living with HIV, leads to overtreatment. We evaluated whether HPV type restriction and more stringent cutoffs on Xpert HPV optimise performance characteristics of this assay for screen and treat.
Methods
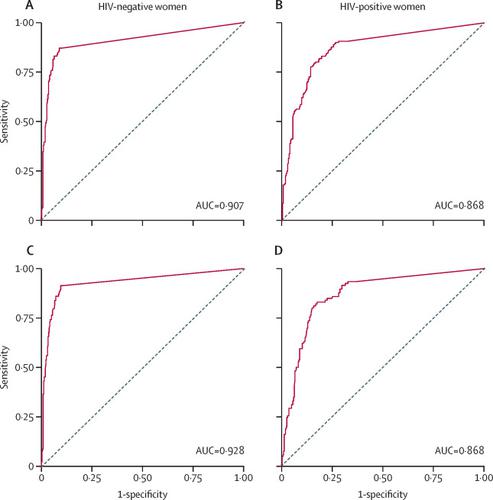
We recruited HIV-negative and HIV-positive women aged 30–65 years from a primary care facility and a referral colposcopy clinic in Cape Town, South Africa. Women included had no history of any anogenital cancer or treatment for cervical dysplasia, had no hysterectomy, and were not pregnancy at the time of recruitment. All women had cervical samples collected for Xpert HPV (an assay that detects high-risk HPV types in five channels: HPV type 16; HPV types 18 or 45, or both; HPV types 31, 33, 35, 52, or 58, or more than one of these types; HPV types 51 or 59, or both; and HPV types 39, 56, 66, or 68, or more than one of these types) and underwent colposcopy and histological sampling with consensus pathology review. Logistic regression and receiver operating characteristic curves were used to evaluate improvements in specificity attained by modifying cycle threshold cutoffs to define screen-positive results.
Results
We recruited 1121 women aged 30–65 years, 586 of whom were HIV-negative and 535 HIV-positive. Sensitivity of detecting cervical intraepithelial neoplasia grade 2 or greater in HIV-negative women using manufacturer-defined cycle threshold cutoffs for all channels was 88·7% (95% CI 83·1–94·3), and specificity was 86·9% (83·4–90·4). Sensitivity was 93·6% (90·0–97·3) and specificity 59·9% (54·1–65·7) in HIV-positive women. Cycle threshold values from channels detecting HPV type 16, HPV types 18 or 45 (or both), and HPV types 31, 33, 35, 52, or 58 (or more than one of these types) were informative to predict cervical intraepithelial neoplasia grade 2 or greater. Shifting cycle threshold cutoffs on these three channels allowing sensitivity to decline to 75–85%, led to specificities of 91·3–95·3% in HIV-negative women and 77·0–85·8% in HIV-positive women.
Interpretation
More stringent cycle threshold cutoffs on selected channels in Xpert HPV improve specificity with only modest losses in sensitivity, making this assay an optimal choice for HPV-based screen and treat in settings with a high prevalence of HIV. These modifications can be made from standard output with no need for new engineering. Decision making about performance characteristics of HPV testing can be shifted to programme implementers and cutoffs selected according to resource availability and community preferences.
Funding
Supported by the National Cancer Institute UH2/3 CA189908.
中文翻译:

对人乳头瘤病毒检测进行修改以优化其在资源匮乏环境中进行宫颈癌筛查的效用的临床评估:一项诊断准确性研究。
背景
基于 HPV 的筛查和治疗是在资源匮乏地区进行宫颈癌筛查的推荐方法,但人乳头瘤病毒 (HPV) 检测的特异性非常低,尤其是在感染 HIV 的女性中,会导致过度治疗。我们评估了 Xpert HPV 的 HPV 类型限制和更严格的截止值是否优化了该检测筛选和治疗的性能特征。
方法
我们从南非开普敦的初级保健机构和转诊阴道镜诊所招募了年龄在 30-65 岁之间的 HIV 阴性和 HIV 阳性女性。纳入的女性没有任何肛门生殖器癌症或宫颈发育不良治疗史,没有子宫切除术,并且在招募时没有怀孕。所有女性都收集了 Xpert HPV 的宫颈样本(一种检测高危 HPV 类型的检测方法,可通过以下五个通道进行:HPV 16 型;HPV 18 或 45 型,或两者;HPV 31、33、35、52 或 58 型,或这些类型中的一种以上;HPV 51 型或 59 型,或两者;以及 HPV 39、56、66 或 68 型,或这些类型中的一种以上),并接受了阴道镜检查和组织学取样,并进行了共识病理学审查。
结果
我们招募了 1121 名 30-65 岁的女性,其中 586 名 HIV 阴性,535 名 HIV 阳性。使用制造商定义的所有通道的周期阈值截止值检测 HIV 阴性女性宫颈上皮内瘤变 2 级或更高的敏感性为 88·7% (95% CI 83·1–94·3),特异性为 86·9% (83·4–90·4)。HIV 阳性女性的敏感性为 93·6% (90·0–97·3),特异性为 59·9% (54·1-65·7)。来自检测 HPV 16 型、18 或 45 型(或两者)和 HPV 31、33、35、52 或 58 型(或这些类型中的一种以上)的通道的周期阈值可提供预测宫颈上皮内瘤变分级的信息2 或更大。改变这三个通道的循环阈值,使敏感性下降到 75-85%,导致 HIV 阴性女性的特异性为 91·3-95·3%,HIV 阳性女性的特异性为 77·0-85·8%。
解释
Xpert HPV 中选定通道的更严格的循环阈值截止值提高了特异性,而灵敏度只有适度的损失,使该检测成为基于 HPV 筛查和治疗的最佳选择,在 HIV 流行率高的环境中。这些修改可以从标准输出进行,不需要新的工程。关于 HPV 检测性能特征的决策可以转移到根据资源可用性和社区偏好选择的项目实施者和截止点。
资金
由美国国家癌症研究所 UH2/3 CA189908 支持。


























 京公网安备 11010802027423号
京公网安备 11010802027423号