当前位置:
X-MOL 学术
›
Gastroenterology
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
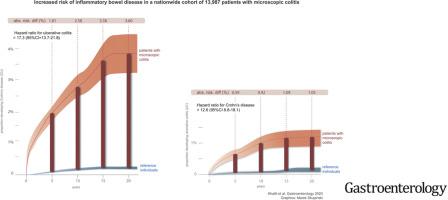
Microscopic Colitis and Risk of Inflammatory Bowel Disease in a Nationwide Cohort Study.
Gastroenterology ( IF 29.4 ) Pub Date : 2020-01-08 , DOI: 10.1053/j.gastro.2019.12.028 Hamed Khalili 1 , Kristin E Burke 2 , Bjorn Roelstraete 3 , Michael C Sachs 4 , Ola Olén 5 , Jonas F Ludvigsson 6
Gastroenterology ( IF 29.4 ) Pub Date : 2020-01-08 , DOI: 10.1053/j.gastro.2019.12.028 Hamed Khalili 1 , Kristin E Burke 2 , Bjorn Roelstraete 3 , Michael C Sachs 4 , Ola Olén 5 , Jonas F Ludvigsson 6
Affiliation
|
BACKGROUND & AIMS
Microscopic colitis shares pathogenetic mechanisms with inflammatory bowel disease (IBD). We studied the association between microscopic colitis and risk of incident IBD using data from a nationwide cohort study.
METHODS
We conducted a prospective cohort study of all adults who received a diagnosis of microscopic colitis from 1990 through 2017 in Sweden and risk of incident IBD. Cases of microscopic colitis (n= 13,957) were identified through Systematized Nomenclature of Medicine codes from the ESPRESSO (Epidemiology Strengthened by histoPathology Reports in Sweden) study, which included gastrointestinal pathology reports from all of Sweden's 28 centers. Individuals with microscopic colitis were matched to 5 general population controls (n = 66,820) and to unaffected siblings (n =13,943). Cox regression was used to estimate adjusted hazard ratio (aHRs) and 95% confidence intervals (CIs).
RESULTS
Through December of 2017, we identified 323 incident cases of ulcerative colitis (UC) and 108 incident cases of Crohn's disease (CD) in patients with microscopic colitis compared with 94 UC and 42 CD cases in population comparators. Mean times from diagnosis of microscopic colitis to diagnosis of CD was 3.3 ± 3.2 years and to diagnosis of UC was 3.2 ± 3.5 years. In multivariable models, microscopic colitis was associated with an aHR of 12.6 (95% CI 8.8-18.1) for CD, 17.3 (95% CI 13.7-21.8) for UC, and 16.8 (95% CI 13.9-20.3) for IBD. The 10-year absolute excess risks of CD and UC were 0.9 (95% CI 0.7-1.1) and 2.6 (95% CI 2.2-2.9) percentage points, respectively. In sensitivity analyses, comparing patients with microscopic colitis with their unaffected siblings, the aHRs of CD and UC were 5.4 (95% CI 3.2-9.2) and 9.4 (95% CI 6.4-13.8), respectively.
CONCLUSIONS
In a population-based study in Sweden, we found a significant increase in risk of incident IBD among patients with microscopic colitis. Future studies should focus on potential mechanisms underlying these observed associations.
中文翻译:

一项全国性队列研究显示,显微镜下的结肠炎和肠炎的风险。
背景与目的显微结肠炎与炎症性肠病(IBD)具有共同的发病机制。我们使用一项全国性队列研究的数据研究了微观结肠炎与IBD发病风险之间的关系。方法我们对1990年至2017年在瑞典被诊断出患有微观结肠炎且发生IBD风险的所有成年人进行了一项前瞻性队列研究。通过ESPRESSO(瑞典流行病学由瑞典组织病理学报告加强)研究的系统化医学命名法鉴定了微观结肠炎(n = 13957),其中包括瑞典28个中心的胃肠道病理学报告。患有显微镜性结肠炎的个体与5个一般人群对照(n = 66,820)和未受影响的兄弟姐妹(n = 13,943)匹配。使用Cox回归估计调整后的危险比(aHRs)和95%置信区间(CIs)。结果截至2017年12月,我们在微观结肠炎患者中鉴定出323例溃疡性结肠炎(UC)病例和108例克罗恩病(CD)病例,而在人群比较者中则为94 UC和42例CD病例。从诊断微观结肠炎到诊断CD的平均时间为3.3±3.2年,而诊断为UC的平均时间为3.2±3.5年。在多变量模型中,微观结肠炎的CD的aHR为12.6(95%CI 8.8-18.1),UC的aHR为17.3(95%CI 13.7-21.8),IBD的aHR为16.8(95%CI 13.9-20.3)。CD和UC的10年绝对绝对风险分别为0.9(95%CI 0.7-1.1)和2.6(95%CI 2.2-2.9)个百分点。在敏感性分析中,通过比较未患病的微观结肠炎患者,CD和UC的aHR分别为5.4(95%CI 3.2-9.2)和9.4(95%CI 6.4-13.8)。结论在瑞典的一项基于人群的研究中,我们发现微观结肠炎患者发生IBD的风险显着增加。未来的研究应关注这些观察到的关联的潜在机制。
更新日期:2020-01-08
中文翻译:

一项全国性队列研究显示,显微镜下的结肠炎和肠炎的风险。
背景与目的显微结肠炎与炎症性肠病(IBD)具有共同的发病机制。我们使用一项全国性队列研究的数据研究了微观结肠炎与IBD发病风险之间的关系。方法我们对1990年至2017年在瑞典被诊断出患有微观结肠炎且发生IBD风险的所有成年人进行了一项前瞻性队列研究。通过ESPRESSO(瑞典流行病学由瑞典组织病理学报告加强)研究的系统化医学命名法鉴定了微观结肠炎(n = 13957),其中包括瑞典28个中心的胃肠道病理学报告。患有显微镜性结肠炎的个体与5个一般人群对照(n = 66,820)和未受影响的兄弟姐妹(n = 13,943)匹配。使用Cox回归估计调整后的危险比(aHRs)和95%置信区间(CIs)。结果截至2017年12月,我们在微观结肠炎患者中鉴定出323例溃疡性结肠炎(UC)病例和108例克罗恩病(CD)病例,而在人群比较者中则为94 UC和42例CD病例。从诊断微观结肠炎到诊断CD的平均时间为3.3±3.2年,而诊断为UC的平均时间为3.2±3.5年。在多变量模型中,微观结肠炎的CD的aHR为12.6(95%CI 8.8-18.1),UC的aHR为17.3(95%CI 13.7-21.8),IBD的aHR为16.8(95%CI 13.9-20.3)。CD和UC的10年绝对绝对风险分别为0.9(95%CI 0.7-1.1)和2.6(95%CI 2.2-2.9)个百分点。在敏感性分析中,通过比较未患病的微观结肠炎患者,CD和UC的aHR分别为5.4(95%CI 3.2-9.2)和9.4(95%CI 6.4-13.8)。结论在瑞典的一项基于人群的研究中,我们发现微观结肠炎患者发生IBD的风险显着增加。未来的研究应关注这些观察到的关联的潜在机制。


























 京公网安备 11010802027423号
京公网安备 11010802027423号