Journal of Neuroradiology ( IF 3.5 ) Pub Date : 2019-11-10 , DOI: 10.1016/j.neurad.2019.10.003 Yeonah Kang , Kuo-Chen Wei , Cheng Hong Toh
|
Purpose
To evaluate the potential of quantitative dynamic susceptibility contrast (DSC) perfusion MR imaging parameters as imaging biomarkers for predicting intraoperative blood loss in meningioma.
Methods
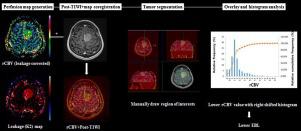
Fifty-one non-embolized meningioma patients who had undergone preoperative DSC perfusion MR imaging were retrospectively included. The corrected relative cerebral blood volume (rCBV) and leakage coefficient (K2) of the entire enhanced tumor were obtained using leakage correction. Tumor volume, location, grade, and other clinical variables, were also analyzed. To investigate the vascularity and vascular permeability of meningiomas, and their correlation with predicting estimated blood loss (EBL) using preoperative DSC perfusion MR imaging, the authors proposed an index reflecting the inherent tendency of meningiomas to bleed after controlling volume (i.e., EBL/cm3). Simple regression was performed to identify predictors of EBL/cm3; subsequently, the relevant variables included in the stepwise multiple linear regression.
Results
On univariate analysis, EBL/cm3 was correlated with rCBV (r = 0.677; P < 0.001), K2 (r = 0.294; P = 0.036), and tumor volume (r = –0.312, P = 0.026). EBL/cm3 was not correlated with age (P = 0.873), sex (P = 0.404), tumor location (P = 0.327), or histological grade (P = 0.230). On multiple linear regression, rCBV (β = 0.663 [0.463–0.864], B = 1.293 [0.903–1.684; P < 0.001) and K2 (β = 0.260 [0.060–0.460], B = 2.277 [0.523–4.031], P = 0.012), were the only independent predictors of EBL/cm3.
Conclusion
The rCBV and K2 derived from DSC perfusion MR imaging in meningiomas may serve as feasible tools for clinicians to predict intraoperative blood loss and facilitate surgical planning.
中文翻译:

我们可以预测脑膜瘤患者的术中失血量吗?动态磁化率对比增强磁共振成像的应用
目的
评估定量动态磁敏感对比 (DSC) 灌注 MR 成像参数作为预测脑膜瘤术中失血的成像生物标志物的潜力。
方法
回顾性纳入了 51 名接受术前 DSC 灌注 MR 成像的非栓塞脑膜瘤患者。使用渗漏校正获得整个增强肿瘤的校正相对脑血容量(rCBV)和渗漏系数(K 2)。还分析了肿瘤体积、位置、等级和其他临床变量。为了研究脑膜瘤的血管分布和血管通透性,以及它们与使用术前 DSC 灌注 MR 成像预测估计失血量 (EBL) 的相关性,作者提出了一个反映脑膜瘤在控制体积后出血的内在趋势的指数(即 EBL/cm 3)。进行简单回归以确定 EBL/cm 3 的预测因子; 随后,将相关变量纳入逐步多元线性回归。
结果
在单变量分析中,EBL/cm 3与 rCBV ( r = 0.677;P < 0.001)、K 2 ( r = 0.294;P = 0.036) 和肿瘤体积 ( r = –0.312,P = 0.026) 相关。EBL/cm 3与年龄(P = 0.873)、性别(P = 0.404)、肿瘤位置(P = 0.327)或组织学分级(P = 0.230)无关。在多元线性回归中,rCBV ( β = 0.663 [0.463–0.864], B = 1.293 [0.903–1.684; P < 0.001) 和 K 2 ( β = 0.260 [0.060–0.460], B = 2.277 [0.523–4.031], P = 0.012) 是 EBL/cm 3的唯一独立预测因子。
结论
来自脑膜瘤 DSC 灌注 MR 成像的 rCBV 和 K 2可作为临床医生预测术中失血量和促进手术计划的可行工具。



























 京公网安备 11010802027423号
京公网安备 11010802027423号