Trial of Early Minimally Invasive Removal of Intracerebral Hemorrhage
Abstract
Background
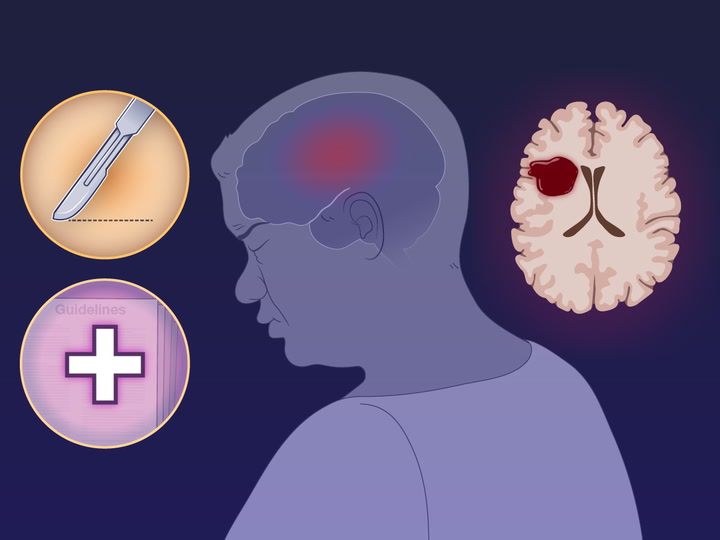
Trials of surgical evacuation of supratentorial intracerebral hemorrhages have generally shown no functional benefit. Whether early minimally invasive surgical removal would result in better outcomes than medical management is not known.
Methods
In this multicenter, randomized trial involving patients with an acute intracerebral hemorrhage, we assessed surgical removal of the hematoma as compared with medical management. Patients who had a lobar or anterior basal ganglia hemorrhage with a hematoma volume of 30 to 80 ml were assigned, in a 1:1 ratio, within 24 hours after the time that they were last known to be well, to minimally invasive surgical removal of the hematoma plus guideline-based medical management (surgery group) or to guideline-based medical management alone (control group). The primary efficacy end point was the mean score on the utility-weighted modified Rankin scale (range, 0 to 1, with higher scores indicating better outcomes, according to patients’ assessment) at 180 days, with a prespecified threshold for posterior probability of superiority of 0.975 or higher. The trial included rules for adaptation of enrollment criteria on the basis of hemorrhage location. A primary safety end point was death within 30 days after enrollment.

Results
A total of 300 patients were enrolled, of whom 30.7% had anterior basal ganglia hemorrhages and 69.3% had lobar hemorrhages. After 175 patients had been enrolled, an adaptation rule was triggered, and only persons with lobar hemorrhages were enrolled. The mean score on the utility-weighted modified Rankin scale at 180 days was 0.458 in the surgery group and 0.374 in the control group (difference, 0.084; 95% Bayesian credible interval, 0.005 to 0.163; posterior probability of superiority of surgery, 0.981). The mean between-group difference was 0.127 (95% Bayesian credible interval, 0.035 to 0.219) among patients with lobar hemorrhages and −0.013 (95% Bayesian credible interval, −0.147 to 0.116) among those with anterior basal ganglia hemorrhages. The percentage of patients who had died by 30 days was 9.3% in the surgery group and 18.0% in the control group. Five patients (3.3%) in the surgery group had postoperative rebleeding and neurologic deterioration.
Conclusions
Among patients in whom surgery could be performed within 24 hours after an acute intracerebral hemorrhage, minimally invasive hematoma evacuation resulted in better functional outcomes at 180 days than those with guideline-based medical management. The effect of surgery appeared to be attributable to intervention for lobar hemorrhages. (Funded by Nico; ENRICH ClinicalTrials.gov number, NCT02880878.)
Notes
This article was updated on April 11, 2024, at NEJM.org.
A data sharing statement provided by the authors is available with the full text of this article at NEJM.org.
Supported by Nico (Indianapolis).
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
We thank the staff at the Neurological Emergency Treatment Trials Network for providing access to training and certification with respect to the modified Rankin scale; the members of the data and safety monitoring board (Drs. Mark Hadley, Gregory Campbell, and Opeolu Adeoye), with special thanks in memoriam to Dr. Campbell who provided the critical role of biostatistician; and especially to all our patients, their families, and the clinicians who made the trial possible.
Supplementary Material
Research Summary (nejmoa2308440_research-summary.pdf)
- Download
- 577.25 KB
Protocol (nejmoa2308440_protocol.pdf)
- Download
- 9.96 MB
Supplementary Appendix (nejmoa2308440_appendix.pdf)
- Download
- 2.02 MB
Disclosure Forms (nejmoa2308440_disclosures.pdf)
- Download
- 2.46 MB
Data Sharing Statement (nejmoa2308440_data-sharing.pdf)
- Download
- 70.65 KB
Information & Authors
Information
Published In
Copyright
Copyright © 2024 Massachusetts Medical Society. All rights reserved.
History
Published online: April 10, 2024
Published in issue: April 11, 2024
Topics
Authors
Affiliations
From the Departments of Neurosurgery (G. Pradilla, J.A.G., D.L.B.), Emergency Medicine (J.J.R., A.J.H., D.W.W.), Neurology (J.J.R., J.W.A., M. Frankel), and Radiology (J.W.A., X.T.L.), Emory University School of Medicine, and the Marcus Stroke and Neuroscience Center, Grady Memorial Hospital (G. Pradilla, J.J.R., A.J.H., J.A.G., M. Frankel, D.W.W.) — both in Atlanta; Berry Consultants, Austin, TX (B.R.S., G. Paulon, A.M., R.J.L., M. Fitzgerald); the Department of Biostatistics, Vanderbilt University School of Medicine, Nashville (B.R.S.); the Department of Emergency Medicine, Harbor–UCLA Medical Center, Torrance, CA (R.J.L.); the Department of Psychiatry, University of Michigan, Ann Arbor (A.F.C.); the Cerebrovascular Center, Cleveland Clinic, Cleveland (M.B., J.G.); the Department of Neurosurgery, University of Pennsylvania, Philadelphia (B.J.); the Department of Neurological Surgery, University of Pittsburgh, Pittsburgh (G.Z.); the Department of Neurology, Brigham and Women’s Hospital, Boston (B.J.M.); the Department of Neurosurgery, State University of New York at Buffalo, Buffalo (J.D., A.S.); the Department of Neurosurgery, University of Missouri, Columbia (M.R.C.), and the Department of Neurology, Washington University, St. Louis (S.G.K.); and the Departments of Neurosurgery (M.V.S., B.N.B.) and Pulmonary and Critical Care Medicine (R.S.), Indiana University, Indianapolis.
Metrics & Citations
Metrics
Altmetrics
Citations
Export citation
Select the format you want to export the citation of this publication.
Cited by
- New Hope for Adults with Lobar Intracerebral Hemorrhage, New England Journal of Medicine, 390, 14, (1328-1329), (2024)./doi/full/10.1056/NEJMe2401643
Loading...