Abstract
With increasing possibilities of multi-year missions in deep space, colonizing other planets, and space tourism, it is important to investigate the effects of space travel on human reproduction. This study aimed to systematically review and summarize the results of available literature on space travel, microgravity, and space radiation, or Earth-based spaceflight analogues impact on female and male reproductive functions in humans. This systematic review was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines and Space Biomedicine Systematic Review methods. The search was performed using three databases: PubMed, Web of Science, and Medline Complete. During the database search, 364 studies were identified. After the study selection process, 16 studies were included in the review. Five studies included female participants, and the findings show an increased risk of thromboembolism in combined oral contraceptive users, decreased decidualization, functional insufficiency of corpus luteum, and decreased progesterone and LH levels related to space travel or its simulation. Male participants were included in 13 studies. In males, reproductive health considerations focused on the decrease in testosterone and sex hormone-binding globulin levels, the ratio of male offspring, sperm motility, sperm vitality, and the increase in sperm DNA fragmentation related to space travel or its simulation. Results of this systematic review highlight the need to focus more on the astronaut’s reproductive health in future research, as only 16 studies were found during the literature search, and many more research questions related to reproductive health in astronauts still need to be answered.
Similar content being viewed by others
Introduction
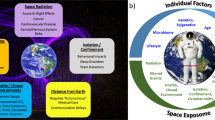
To undertake multi-year missions in deep space, colonize other planets, and/or prepare appropriate safety measures for space tourism, it is important to investigate the possible effects of space travel on human reproduction. During space travel, astronauts are exposed to several hazardous factors, such as alterations in gravitation forces, including hypogravity and hypergravity, or ionizing radiation1,2. Exposure to microgravity has been demonstrated to impair the endocrine system in males3, muscle mass, and bone mass4,5; it also leads to altered fluid and electrolyte balance, cardiovascular changes, or increased glomerular filtration rate in both genders2. Experimental bed rest studies are typically used in humans to simulate spaceflight microgravity6. For in vitro samples, clinostat or random positioning machines are used to simulate microgravity by randomization of the gravity direction over time. In animal studies, hindlimb suspension is usually used to stimulate the physiological effects of microgravity2. Ionizing radiation, which is about 500 times greater in space compared to Earth conditions, was observed to cause DNA damage, apoptosis in ovarian follicles, and sperm DNA fragmentation in animal models1,2,7,8.
Until now, limited research has focused on the effect of space travel on the reproductive system and its function, along with endocrine regulation of reproduction or prenatal development. Endocrine regulation of sex hormones is the most investigated as it also impacts musculoskeletal health and skeletal muscle protein metabolism (e.g.9,10). Most of this research is based on animal models1,2.
Female mouse models show that microgravity affects embryonic stem cell growth and differentiation11, resulting in impaired decidualization of the endometrium needed for implantation and maintaining pregnancy12. Data from therapeutic radiation on ovaries suggests that space radiation exposure during a typical Mars mission may reduce the ovarian reserve by 50% by destroying some of the primordial follicles. Furthermore, space radiation may lead to a decreased time interval to menopause, leading to a decreased reproductive capacity of the female astronaut13. Exposure to total body radiation of 15 Gy leads to the loss of ovarian function in humans14.
In males, the microgravity exposure was observed to reduce the total sperm count in mice models15, decrease testes weight, and decrease testosterone concentrations in male rats2,16. Exposure to ionizing radiation increases sperm DNA fragmentation in Echinogammarus marinus models7, affecting the male reproductive health. Data from therapeutic radiation on testes in humans show that a dose higher than 1 Gy might result in azoospermia and risk for hereditary disorders17. Furthermore, decreased serum testosterone levels were observed in men treated with radiotherapy for rectal cancer when testes are exposed to direct or scattered radiation18.
As described in The Impact of Sex and Gender on Adaptation to Space: A NASA Decadal Review19, reproductive demographics of female and male US astronauts significantly differ based on biological processes and gender roles for parents. Women are usually the primary caregivers (e.g., ref. 20) and are often required to take an extended family leave from their career when having a child (e.g., ref. 21). A smaller number of female astronauts (44.7%) have at least one child compared to the male astronauts (83.9%). Female astronauts also significantly delay reproduction, on average, by 5.6 years compared to males. It was hypothesized that the delayed reproduction in female astronauts is related to the required extensive space travel training time19. A new NASA decadal review is expected next year, adding more current data on the topic. However, not only delayed reproduction but also the impact of the potential acceleration of aging and gonadal radiation exposure related to space travel might be other factors affecting the reproduction capacity in female astronauts19. Therefore, the aim of this study was to systematically review and summarize the results of available literature on space travel, microgravity, and space radiation’s impact on female and male reproductive functions in humans.
Results
Characteristics of included studies
During the database search, 364 studies were identified (Pubmed: 121 articles; Medline Complete: 142 articles; Web of Science: 101 articles). After the duplicate removal (n = 160), studies involving animal samples (n = 45), different methodologies, or non-English language articles (e.g., conference paper, book chapter; n = 12), 147 studies were screened based on title and abstract in which 120 studies were excluded. In the last stage, 27 studies remained, followed by the exclusion of 5 studies due to no full-text being available and eight studies because the outcomes needed to match the topic. Via another method (accidental find), two studies focusing on ionizing radiation’s effect on male reproductive health were found22,23. A total of 16 studies were included in the systematic review.
The methodological quality of the included studies (Table 1) ranged from 70.0%24 to 90.9%25, suggesting good methodological quality26. The most common methodological deficits consisted of not reporting the study’s hypothesis clearly, not reporting the probability values, and the lack of representativeness of the source population. The methodological quality of the included studies is shown in Supplementary Table 1.
Six of the included studies used bed rest study design. Bed rest studies’ methodological quality (Table 2) ranged between 227 to 7 points28. No study indicated a prohibition of sunlight exposure. Four studies did not indicate a set wake/sleep time6,10,29,30. One study design allowed a limited ambulation time (to shower and toilet)29. In three of the included studies, the recommended 6° head-down tilt was not used6,27,29.
Articles meeting the inclusion criteria included four articles from USA (25%), two articles from China (12, 5%), two articles from Russia (12, 5%), one article from Poland (6, 25%), one article from Italy (6, 25%), one article from South Korea (6, 25%), one article from India (6, 25%), one article from Japan (6, 25%), one article from Spain (6, 25%), one article from Austria (6, 25%), and one article from Germany (6, 25%)6,10,12,22,23,24,25,27,28,29,30,31,32,33,34,35.
As shown in Table 3, in most of the included studies, only male participants were analyzed (11 studies; 68, 75%6,10,22,23,25,28,29,30,31,33,35), three studies focused on female participants (18, 75%12,24,32), and two studies included a mixed sample (12, 5%27,34).
Thirteen articles reported data from the experiments on Earth. Simulated microgravity by parabolic flight was used in two studies31,35 and by clinostat system in one study12; in two studies ionizing radiation occupational exposure was used22,23, head-down bed rest was performed in four studies10,27,28,30, bed rest was conducted in two studies6,29, in two studies dry immersion was used24,32, and in one study data from water submersion were reported25. Three articles reported data on space exposure30,33,34. Eight of included studies focused on endocrine changes after the space flight or its simulation10,25,6,27,28,29,30; four studies focused on sperms22,23,31,35; two studies focused on menstrual cycle changes24,32; one study focused on endometrial stromal cells12, one study focus of the venous thromboembolism risk34, and one study focused on offspring sex ratio in male astronauts33.
Female and mixed studies
Three studies, including female participants, and two studies, including mixed samples, were identified during the study selection process. Their characteristics are shown in Table 4. One study used a clinostat system to simulate the microgravity of in vitro samples of human endometrial stromal cells (PSCs) from the uterus12. Two studies used dry immersion to simulate microgravity; in both studies, participants were allowed 30 min/day to spend outside the immersion bath for hygiene procedures24,32. Tomilovskaya et al.32 described the first female dry immersion study, and their participants were involved in their study for two menstrual cycles. The three-day dry immersion occurred between day 7 and day 10 of participants’ menstrual cycles32. In a study by Gorbacheva et al.24, two menstrual cycles were followed; the 5-day-long dry immersion was performed between day 10 and day 15 of participants’ menstrual cycles. One study used one hour-long -12° head-down bed rest to simulate microgravity and analyze endocrine parameter changes27. In one study, spaceflight exposure was used to analyze proteins involved in clotting cascade from blood samples obtained twice before spaceflight, five times during the flight, and twice after flight34.
In Table 5, results from female and mixed samples studies are shown. In female in vitro samples, exposure to microgravity was observed to decrease decidualization (the process of endometrial cells in preparation for, or during pregnancy) by decreasing proliferation and migration and endometrial stromal cells growth rate through Akt/MMP and FOXO3a/autophagic flux12. Two studies reported that menstrual cycle length stayed intact after dry immersion exposure24,32. Gorbacheva et al.24 observed decreased luteinizing hormone (LH), progesterone, and ovarian volume at day 9 of the menstrual cycle after the immersion. On the other hand, an increase in dominant follicle diameter and no change in uterus size and endometrial thickness were reported24. The mixed sample study focused on venous thromboembolism risk in male and female astronauts, showing an increased risk in females taking combined oral contraceptives34. A head-down bed rest mixed sample study reported no statistically significant change in oestradiol, testosterone, and LH levels after the rest27.
Male studies
Eleven studies focused on male participants were identified during the study selection process. In Table 6, the male studies’ characteristics are summarized. In the study by Little et al.33, retrospective data from astronauts’ biographies were included in the analysis of offspring ratio. A study by Smith et al.30 focused on the effect of long- and short-duration space flight and −6° head-down bed rest on testosterone levels. In two studies, parabolic flights were used to simulate short-duration microgravity31,35. In a study by Boada et al.35, twenty parabolic flight maneuvers (8.5 s of microgravity for each parabola) were used for frozen sperm samples. In a study by Ikeuchi et al.31, fresh sperm samples underwent ten parabolic flight maneuvers (20 to 25 s of microgravity for each parabola). Occupational low-dose exposure to ionizing radiation while working with radiation in a hospital on sperm characteristics was analyzed in two studies22,23. Four studies analyzed the effect of bed rest or −6° head-down bed rest on testosterone levels10,6,28,29. Studies by Belavy et al.6, Liang et al.28, and Zachwieja et al.10 applied a strict bed rest. Study design by Smorawinski et al.29 provided 20 min/day to ambulate (to shower and toilet). In one study, the effect of water submersion on testosterone levels was analyzed25. In the study by Loder et al.25, divers were allowed to emerge for less than 20 min every 4 hours to urinate, defecate, drink, or undergo medical checks.
One of the studies including male participants in the space study setting (Table 7) focused on the offspring sex ratio, showing a decreased ratio of male offspring (43.75%) in male astronauts33. Furthermore, the study by Little et al.33 observed a decreased male offspring ratio of 38.41% in high G pilots compared to 50.34% in low G pilots. The second study using the space study setting focused on endocrine changes, showing no statistically significant changes in testosterone and sex hormone-binding globulin (SHBG) during or after the short and long-duration space flight. A decrease in total, free, and bioavailable testosterone was observed only on the landing day after the space flight, probably as the transient effect of flight30. One study observed decreased sperm motility after microgravity exposure31, and another study by Boada et al.35 observed no statistically significant change in sperm motility, vitality, or sperm DNA fragmentation after exposure to microgravity. Occupational ionizing radiation exposure was observed to decrease sperm motility, vitality, and concentration and to increase sperm DNA fragmentation in comparison with non-exposed controls22,23. Bed rest and head-down bed rest studies show no statistically significant change in testosterone and prolactin after the rest10,28,29,30. SHBG was observed to decrease after the bed rest6. After the water submersion, a decrease in plasma testosterone was observed25.
Discussion
The aim of this study was to systematically review and summarize the results of available literature on space travel, microgravity, and space radiation impact on female and male reproductive functions in humans. The reproductive health consideration of space travel differs for female and male astronauts. In female astronauts, they include oral contraceptive use34, progesterone and LH levels27, ovarian and uterus changes24, decidualization, and endometrial stromal cell growth rate12. In males, reproductive health considerations focus on testosterone and SHBG levels10,25,6,27,28,29,30, the ratio of male offspring33, sperm motility22,23,31,35, sperm vitality22,35, and sperm DNA fragmentation22,23,35. To support those considering these options, it might be helpful to explore assisted reproductive technologies such as oocyte and sperm cryopreservation, along with reproductive counseling possibilities, as suggested by Rose13 and Ronca et al.36.
In female astronauts, the endocrine regulation of the menstrual cycle involves the hypothalamic release of gonadotropin-releasing hormone, which stimulates the pituitary gland to produce follicle-stimulating hormone and luteinizing hormone, which peaks mid-cycle and invokes ovulation37. The developing ovum in ovaries produces estrogen, and the corpus luteum, which forms after ovulation, produces progesterone. Animal models show a decrease in luteinizing hormone related to 37 days-long spaceflights; however, no changes in estrous cycle stages were observed38. In naturally cycling women, simulated microgravity by dry immersion led to a decrease in luteinizing hormone by 12% and progesterone by 52%, showing functional insufficiency of corpus luteum24. The menstrual cycle length was not altered after 3 and 5 days of dry immersion24,32. One hour of −12° head-down bed rest did not induce any significant changes in the endocrine regulation of the cycle, suggesting that longer microgravity exposure is needed to affect the endocrine regulation of the menstrual cycle27. Despite the fact that abnormal uterine bleeding is a common complaint among reproductive-aged women39, uterine bleeding changes were not analyzed in any of the included studies.
As the menstrual bleeding flow management during space flight training and the space flight can be challenging, medically induced amenorrhea using combined oral contraceptives is often used by female astronauts40. However, combined (progestin and estrogen) oral contraceptives were associated with lower circulating concentrations of albumin, higher concentrations of transferrin, and elevated markers of inflammation, which can contribute to an increased risk of venous thromboembolism event during space travel34. The occlusive deep venous thrombosis was diagnosed in one female astronaut during a long-duration spaceflight41, highlighting the need to carefully consider the type of combined oral contraceptives used before and during flight34.
Human pregnancy is currently contradicted during space flight as a safety measure to protect the fetus13,42,43. Multi-year duration space flights and colonization will require understanding the impact of space flight on pregnancy, and simulation studies will try to provide better insight into reproduction in space. Fetal development, long-term effects on gestation under space conditions, and monitoring the development and function of offspring conceived and developed in space are some of the potential priorities for future space programs as described in a European perspective of human development and reproduction in space by Jain et al.43. The study by Cho et al.12 showed that exposure to simulated microgravity leads to decreased decidualization and endometrial stromal cells growth rate due to decrease in Akt activity and FOX03a expression leading to an unreceptive endometrium. Furthermore, if microgravity and space radiation alter the pro-oxidant/antioxidant balance during pregnancy, it can increase the risk of miscarriage, preterm birth, or fetal growth restriction44. The absence of gravitational loading during the last trimester of gestation may cause hypotrophy of muscles and osteopenia in the trunk and legs, leading to delayed acquisition of developmental milestones such as sitting or walking of the fetus developed in space45. Animal models show increased perinatal morbidity for the rats that spent 9 to 20 days in spaceflight during their gestation. In surviving offspring, no delay in walking acquisition was observed46.
High-altitude airplane flights, e.g., transatlantic flights, constitute trivial cosmic radiation exposure for casual travelers. Pregnant pilots, flight attendants, and frequent flyers may exceed the recommended radiation exposure47. During transatlantic air travel in the third trimester of pregnancy, most of the pregnant women report no change in fetal movements during take-off or flight48. A study by Grajewski et al.49 focusing on miscarriage risk among flight attendants shows that cosmic radiation exposure of 0,1 mGy or more may be associated with an increased risk of miscarriage in weeks 9 to 13. However, the miscarriage risk was also associated with other factors such as work during sleep hours and high physical demands, and the miscarriage risk was not increased among flight attendants compared to a control group of teachers49. Maternal stress and exposure to stressful events during pregnancy were observed to impact the infant’s physical health50, premature birth, and low birth weight51, suggesting a possible negative effect of space travel-related stress on the fetus.
Space travel may increase the carcinogenic risk to reproductive organs. This risk was proposed to be higher in women as they have a higher incidence of radiation-induced cancers, as widely discussed in Market al.19. Still, the low number of female astronauts does not allow for assessment of the risk of spaceflight on gynecological cancer36.
In expert opinion by Rose13, significantly reduced ovarian reserve and consequent decrease in the reproductive capacity and decreased time interval to menopause caused by space radiation was suggested in female astronauts. Unfortunately, no original article showing the data about reproductive capacity or age of menopause in astronauts was found during the literature search in this systematic review.
Testosterone is the key hormone in the development of the male reproductive system and promotes muscle and bone mass52. Testosterone has been, therefore, often considered as a potential countermeasure for musculoskeletal losses related to space flight (e.g.10). The testosterone level seems unchanged by the space flight or bed rest study settings9,10,6,27,28,30 apart from the transient effects after flight30. A decrease in testosterone levels was observed in a short-term water submersion (41 h) study by Loder et al.25. Similarly, it was hypothesized that the decrease is related to stress effect25. The self-rated sexual drive was reported to temporarily decrease during space flight in male astronauts parallelly to urinary, plasma, and salivary testosterone levels in a study by Strollo et al.53. Similarly, animal studies show a decrease in testosterone levels in simulated microgravity studies caused by a reduction in testicular blood flow related to body fluid shift1.
Prolactin and LH levels did not change during the analog bed rest study27,6. Similarly, no LH and FSH levels change was observed after a 6-week hindlimb suspension in animal models54. Serum SHBG levels were observed to decrease during bed rest in inactive participants. The physical activity load during the bed rest led to stable SHBG levels6. Similarly, no change during or after the space flight in the level of SHBG was observed by Smith et al.30
Results observed by Ikeuchi et al.31 using fresh semen suggest that sperm motility is reduced by microgravity. In a study by Boada et al.35 using frozen semen, no significant change in sperm motility, vitality, or sperm DNA fragmentation was observed compared to Earth condition after a similar parabolic flight experiment as used by Ikeuchi et al.31. These results suggest that the sperm integrity may be protected by cryopreservation during the space flight when transporting male human gametes into space35. Still, chronic occupational exposure to ionizing radiation was observed to have a detrimental effect on sperm motility, vitality, concentration, and DNA fragmentation22,23. Similarly, ionizing radiation and microgravity were observed to increase sperm DNA fragmentation in animal studies1. Furthermore, a decreased sex ratio of male offspring by male astronauts exposed to high G forces was reported by Little et al.33. The authors hypothesized that sperm sex differences in sperm motility and longevity, smaller size, and cytoplasm content in Y sperm were the reason of decreased sex ratio of male offspring as higher G forces may accelerate metabolism in sperm subtracting energy available for travel to the ovum33. However, current knowledge shows no morphological differences between X and Y sperms in humans55. Still, X and Y sperms differences in genetic content may lead to differences in their stress response56. The study by You et al.57 reported that the viability of human Y spermatozoa was lower after exposure to stress (e.g., different temperatures and culture periods) compared to X spermatozoa, which may result in a shift of the offspring sex ratio as observed by Little et al.33. Similarly, low male sex offspring ratio associated with occupational testicular radiation exposure was observed in a previous study58. On the other hand, no association between offspring sex ratio and gonadal irradiation was observed in childhood cancer survivors in a study by Reulen et al.59
Future studies on the effect of space radiation on both fresh and frozen semen samples are needed to assess the possibility of creating a human sperm bank outside the Earth. A study by Wakayama et al.60 analyzed the effect of space radiation on mouse freeze-dried spermatozoa stored for almost six years on the International Space Station. The sperm DNA and fertility were not affected after the storage outside the Earth compared to control preserved on Earth, and the current data show the possibility of storing freeze-dried spermatozoa for more than 200 years in space60.
Among potential priorities identified by Jain et al.43 for future research regarding reproductive aspects of space flight were topics similar to those covered in this systematic review. Additionally, the effect of space travel on libido and the possibility of pregnancy and birth in space were proposed43. Results of this systematic review highlight the need to focus more on both female and male astronauts’ reproductive health in future research, as only 16 studies were found during the literature search, and many more research questions related to reproductive health in female and male astronauts still need to be answered.
There are several limitations of this systematic review. The main limitation is the few included studies and the wide range of reproductive health parameters they focused on. The small sample sizes, different types of populations (healthy volunteers, astronauts), and different methodologies need to be considered when comparing or generalizing the results. The limited number of studies addressing these health concerns underscores the imperative need for future research dedicated to reproductive health in both female and male astronauts.
Methods
Eligibility criteria for selecting studies
A systematic review of the effect of space travel or its simulation, e.g., bed rest studies, microgravity simulation, or dry immersion, on reproductive health in human females and males was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines61 and according the Space Biomedicine Systematic Review methods (https://sites.google.com/view/sr-methods/home). The search was performed using three databases, PubMed, Web of Science, and Medline Complete, on the 29th of April 2023 by one researcher (MG). The eligibility criteria included: (1) astronauts, space travel, or space simulation; (2) experimental or retrospective studies performed on human participants (animal studies were excluded); (3) description of reproductive health parameters.
Search strategy and selection process
The following terms with Boolean operators were used for the search: (“infertility” OR “birth outcomes” OR “amenorrhea” OR “menstrual” OR “menstrual cycle” OR “follicular phase” OR “luteal phase” OR “menstruation” OR “ovarian cycle” OR “ovulation” OR “anovulation” OR “reproduct*” OR “obstetric*” OR “gynecolog*” OR “maternal” OR “pregnan*” OR “contracept*” OR “prenatal” OR “postpartum” OR “preconception” OR “women’s health” OR “miscarriage” OR “pregnancy loss” OR “menarche” OR “polycystic ovary syndrome” OR “menopause” OR “endometriosis” OR “stillbirth” OR “placental abruption” OR “low birth weight” OR “preterm birth” OR “in vitro fertilization” OR “irregular periods” OR “sperm” OR “testosterone” OR “semen quality” OR “oligospermia” OR “semen” OR “testis” OR “testes” OR “testicular” OR “offspring” OR “reproductive hormone” OR “asthenozoospermia” OR “oligozoospermia” OR “oligoasthenozoospermia” OR “oligoasthenoteratozoospermia” OR “teratozoospermia” OR “spermatogenesis” OR “varicocele” OR “erection” OR “libido” OR “erectile dysfunction” OR “sexual drive”) AND (“space travel” OR “astronaut*” OR “spaceflight” OR “space analogue” OR “cosmonaut*” OR “space simulation” OR “zero gravity” OR “microgravity” OR “hypogravity” OR “low gravity” OR “space radiation”) AND (“human” OR “participant*” OR “women” OR “men” OR “woman” OR “man”) NOT (“review”). The literature search did not exclude any studies published before certain data due to a limited number of scientific studies focused on the analyzed topic as proposed in Ahrari et al.1. Studies published until April 2023 were included in this study. Exclusion criteria included animal studies, non-English language, review articles, conference papers, books, and book chapters, and no full-text available. All studies identified in the search were imported into Rayyan systematic review software62 to continue the selection process. Studies that did not meet the inclusion criteria (e.g., duplicates, non-English articles, reviews, conference papers, books and book chapters, and animal studies) were excluded by one researcher (MG). The title and abstract of the remaining studies were screened by two researchers (MG, ACP). Any disagreement between researchers was resolved by discussion. After that, the full texts of the included studies were screened to confirm their relevance to the current systematic review. The PRISMA flow diagram summarizes the study selection process (Fig. 1).
PRISMA flow diagram of the study selection process (template from61).
Data collection process and assessment of study quality
Data extraction was performed by two researchers (MG, MB) using a pre-determined form consisting of (i) study characteristics (author, publication year and country, sample characteristics, study setting: Earth/space, and exposure: spaceflight/microgravity/ionizing radiation/bed rest/water submersion/dry immersion); and (ii) analyzed reproductive health parameters and results.
The methodological quality assessment of included studies was performed by one researcher (MG) using the Downs and Black Quality Assessment Checklist63. The original checklist consists of 27 questions assessing the quality of reporting, external and internal validity, and statistical power. For this review, 13 items were considered relevant. A similar approach was used in previous studies by Gimunová et al.64 and Paludo et al.65. A binary score for each question: 0 = no/unable to determine, 1= yes was used. The final score (in %) was classified as follows: <45.4% “poor” methodological quality; 45.5–61.0% “fair” methodological quality”; and >61.0% “good” methodological quality26. The quality assessment was not used to exclude any study.
Additionally, as recommended in Space Biomedicine Systematic Review Methods, the Bed rest studies transferability was assessed by the recommended tool (https://sites.google.com/view/sr-methods/guides/bed rest-transferability) used in a previous systematic review by Winnard et al.66. The methodological quality of bed rest studies was assessed by one researcher (MG) considering eight questions comparing the study design with “ideal design” resulting in a total score between 0 to 8 points.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The original studies presented in the systematic review are included in the article; further inquiries can be directed to the corresponding author.
References
Ahrari, K., Omolaoye, T. S., Goswami, N., Alsuwaidi, H. & du Plessis, S. S. Effects of space flight on sperm function and integrity: A systematic review. Front Physiol. 13, 904375 (2022).
Mishra, B. & Luderer, U. Reproductive hazards of space travel in women and men. Nat. Rev. Endocrinol. 15, 713–730 (2019).
Macho, L. et al. The response of the endocrine system to stress loads during space flight in human subjects. Adv. Space Res. 31, 1605–1610 (2003).
Narici, M. V. & de Boer, M. D. Disuse of the musculo-skeletal system in space and on Earth. Eur. J. Appl Physiol. 111, 403–420 (2011).
Tanaka, K., Nishimura, N. & Kawai, Y. Adaptation to microgravity, deconditioning, and countermeasures. J. Physiological Sci. 67, 271–281 (2017).
Belavý, D. L. et al. The effects of bed rest and countermeasure exercise on the endocrine system in male adults: evidence for immobilization-induced reduction in sex hormone-binding globulin levels. J. Endocrinol. Invest 35, 54–62 (2012).
Fuller, N., Smith, J. T. & Ford, A. T. Impacts of ionising radiation on sperm quality, DNA integrity and post-fertilisation development in marine and freshwater crustaceans. Ecotoxicol. Environ. Saf. 186, 109764 (2019).
Straume, T., Blattnig, S. R., Blattnig, S. & Zeitlin, C. Radiation Hazards and the Colonization of Mars. https://www.researchgate.net/publication/271092972.
Ferrando, A. A., Lane, H. W., Stuart, C. A., Davis-Street, J. & Wolfe, R. R. Prolonged bed rest decreases skeletal muscle and whole body protein synthesis. Am. J. Physiol.-Endocrinol. Metab. 270, E627–E633 (1996).
Zachwieja, J. J. et al. Testosterone Administration Preserves Protein Balance But Not Muscle Strength during 28 Days of Bed Rest1. J. Clin. Endocrinol. Metab. 84, 207–212 (1999).
Blaber, E. A. et al. Microgravity Reduces the Differentiation and Regenerative Potential of Embryonic Stem Cells. Stem Cells Dev. 24, 2605–2621 (2015).
Cho, H.-J. et al. Microgravity inhibits decidualization via decreasing Akt activity and FOXO3a expression in human endometrial stromal cells. Sci. Rep. 9, 12094 (2019).
Rose, B. I. Female astronauts: Impact of space radiation on menopause. Eur. J. Obstet. Gynecol. Reprod. Biol. 271, 210–213 (2022).
Kim, S.-Y., Kim, S. K., Lee, J. R. & Woodruff, T. K. Toward precision medicine for preserving fertility in cancer patients: existing and emerging fertility preservation options for women. J. Gynecol. Oncol. 27, e22 (2016).
Usik, M. A. & Ogneva, I. V. Cytoskeleton Structure in Mouse Sperm and Testes After 30 Days of Hindlimb Unloading and 12 h of Recovery. Cell. Physiol. Biochem. 51, 375–392 (2018).
Merrill, A. H., Wang, E., Mullins, R. E., Grindeland, R. E. & Popova, I. A. Analyses of plasma for metabolic and hormonal changes in rats flown aboard COSMOS 2044. J. Appl Physiol. 73, S132–S135 (1992).
Mazonakis, M., Damilakis, J., Varveris, H. & Gourtsouiannis, N. Radiation dose to testes and risk of infertility from radiotherapy for rectal cancer. Oncol Rep https://doi.org/10.3892/or.15.3.729 (2006).
Buchli, C., Martling, A., Arver, S. & Holm, T. Testicular Function After Radiotherapy for Rectal Cancer—A Review. J. Sex. Med. 8, 3220–3226 (2011).
Mark, S. et al. The Impact of Sex and Gender on Adaptation to Space: Executive Summary. J. Women’s Health 23, 941–947 (2014).
Cantillo-Medina, C. P., Perdomo-Romero, A. Y. & Ramírez-Perdomo, C. A. Características y experiencias de los cuidadores familiares en el contexto de la salud mental. Rev. Peru. Med Exp. Salud Publica 39, 185–192 (2022).
Grandahl, M., Stern, J. & Funkquist, E.-L. Longer shared parental leave is associated with longer duration of breastfeeding: a cross-sectional study among Swedish mothers and their partners. BMC Pediatr. 20, 159 (2020).
Kumar, D. et al. Semen Abnormalities, Sperm DNA Damage and Global Hypermethylation in Health Workers Occupationally Exposed to Ionizing Radiation. PLoS One 8, e69927 (2013).
Zhou, D. D., Hao, J. L., Guo, K. M., Lu, C. W. & Liu, X. D. Sperm quality and DNA damage in men from Jilin Province, China, who are occupationally exposed to ionizing radiation. Genet. Mol. Res. 15, (2016).
Gorbacheva, E. Y. U. et al. The State of the Organs of the Female Reproductive System after a 5-Day “Dry” Immersion. Int J. Mol. Sci. 24, 4160 (2023).
Loder, I. et al. Adrenomedullin and elements of orthostatic competence after 41 h of voluntary submersion in water as measured in four healthy males. Eur. J. Appl Physiol. 96, 644–650 (2006).
Meignié, A. et al. The Effects of Menstrual Cycle Phase on Elite Athlete Performance: A Critical and Systematic Review. Front Physiol. 12, 654585 (2021).
Strollo, F. et al. A Short Term-12° Head Down Tilt Does Not Mimic Microgravity in Terms of Human Gonadal Function. Microgravity Sci. Technol. XVIII-3/4, (2006).
Liang, X. et al. Changes in the Diurnal Rhythms during a 45-Day Head-Down Bed Rest. PLoS One 7, e47984 (2012).
Smorawiński, J. et al. Effects of 3-day bed rest on physiological responses to graded exercise in athletes and sedentary men. J. Appl Physiol. 91, 249–257 (2001).
Smith, S. M., Heer, M., Wang, Z., Huntoon, C. L. & Zwart, S. R. Long-Duration Space Flight and Bed Rest Effects on Testosterone and Other Steroids. J. Clin. Endocrinol. Metab. 97, 270–278 (2012).
Ikeuchi, T. et al. Human sperm motility in a microgravity environment. Reprod. Med Biol. 4, 161–168 (2005).
Tomilovskaya, E. et al. The First Female Dry Immersion (NAIAD-2020): Design and Specifics of a 3-Day Study. Front Physiol. 12, 661959 (2021).
Little, B. B., Rigsby, C. H. & Little, L. R. Pilot and astronaut offspring: possible G-force effects on human sex ratio. Aviat. Space Environ. Med. 58, 707–709 (1987).
Zwart, S. R., Auñón-Chancellor, S. M., Heer, M., Melin, M. M. & Smith, S. M. Albumin, oral contraceptives, and venous thromboembolism risk in astronauts. J. Appl Physiol. 132, 1232–1239 (2022).
Boada, M. et al. Microgravity effects on frozen human sperm samples. J. Assist Reprod. Genet. 37, 2249–2257 (2020).
Ronca, A. E. et al. Effects of Sex and Gender on Adaptations to Space: Reproductive Health. J. Women’s Health 23, 967–974 (2014).
Günther, V. et al. Changes of salivary estrogen levels for detecting the fertile period. Eur. J. Obstet. Gynecol. Reprod. Biol. 194, 38–42 (2015).
Hong, X. et al. Effects of spaceflight aboard the International Space Station on mouse estrous cycle and ovarian gene expression. NPJ Microgravity 7, 11 (2021).
Munro, M. G., Critchley, H. O. D. & Fraser, I. S. The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions. Int. J. Gynecol. Obstet. 143, 393–408 (2018).
Jain, V. & Wotring, V. E. Medically induced amenorrhea in female astronauts. NPJ Microgravity 2, 16008 (2016).
Auñón-Chancellor, S. M., Pattarini, J. M., Moll, S. & Sargsyan, A. Venous Thrombosis during Spaceflight. N. Engl. J. Med. 382, 89–90 (2020).
Jennings, R. T. & Santy, P. A. Reproduction in the Space Environment. Obstet. Gynecol. Surv. 45, 7–17 (1990).
Jain, V. et al. Human development and reproduction in space—a European perspective. NPJ Microgravity 9, 24 (2023).
Steller, J., Alberts, J. & Ronca, A. Oxidative Stress as Cause, Consequence, or Biomarker of Altered Female Reproduction and Development in the Space Environment. Int J. Mol. Sci. 19, 3729 (2018).
Sekulić, S. R., Lukač, D. D. & Naumović, N. M. The fetus cannot exercise like an astronaut: gravity loading is necessary for the physiological development during second half of pregnancy. Med. Hypotheses 64, 221–228 (2005).
Wong, A. M. & De Santis, M. Rat gestation during space flight: Outcomes for dams and their offspring born after return to Earth. Integr. Physiological Behav. Sci. 32, 322–342 (1997).
Barish, R. J. In-Flight Radiation Exposure During Pregnancy. Obstet. Gynecol. 103, 1326–1330 (2004).
Petrikovsky, B., Terrani, M. & Sichinava, L. Transatlantic Air Travel in the Third Trimester of Pregnancy: Does It Affect the Fetus? Am. J. Perinatol. Rep. 08, e71–e73 (2018).
Grajewski, B. et al. Miscarriage Among Flight Attendants. Epidemiology 26, 192–203 (2015).
Bush, N. R. et al. Maternal Stress During Pregnancy Predicts Infant Infectious and Noninfectious Illness. J. Pediatr. 228, 117–125.e2 (2021).
Lima, S. A. M. et al. Is the risk of low birth weight or preterm labor greater when maternal stress is experienced during pregnancy? A systematic review and meta-analysis of cohort studies. PLoS One 13, e0200594 (2018).
Barbonetti, A., D’Andrea, S. & Francavilla, S. Testosterone replacement therapy. Andrology 8, 1551–1566 (2020).
Strollo, F. et al. The effect of microgravity on testicular androgen secretion. Aviat. Space Environ. Med. 69, 133–136 (1998).
Tash, J. S., Johnson, D. C. & Enders, G. C. Long-term (6-wk) hindlimb suspension inhibits spermatogenesis in adult male rats. J. Appl Physiol. 92, 1191–1198 (2002).
Hossain, A. M., Barik, S. & Kulkarni, P. M. Lack of significant morphological differences between human X and Y spermatozoa and their precursor cells (spermatids) exposed to different prehybridization treatments. J. Androl. 22, 119–123 (2001).
Rahman, M. S. & Pang, M.-G. New Biological Insights on X and Y Chromosome-Bearing Spermatozoa. Front Cell Dev. Biol. 7, 388 (2020).
You, Y.-A. et al. Sex chromosome-dependent differential viability of human spermatozoa during prolonged incubation. Hum. Reprod. 32, 1183–1191 (2017).
Hijikata, Y. et al. Association between occupational testicular radiation exposure and lower male sex ratio of offspring among orthopedic surgeons. PLoS One 16, e0262089 (2021).
Reulen, R. C. et al. Offspring sex ratio and gonadal irradiation in the British Childhood Cancer Survivor Study. Br. J. Cancer 96, 1439–1441 (2007).
Wakayama, S. et al. Evaluating the long-term effect of space radiation on the reproductive normality of mammalian sperm preserved on the International Space Station. Sci. Adv. 7, eabg5554 (2021).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ n71 (2021) https://doi.org/10.1136/bmj.n71.
Ouzzani, M., Hammady, H., Fedorowicz, Z. & Elmagarmid, A. Rayyan—a web and mobile app for systematic reviews. Syst. Rev. 5, 210 (2016).
Downs, S. H. & Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health (1978) 52, 377–384 (1998).
Gimunová, M., Paulínyová, A., Bernaciková, M. & Paludo, A. C. The Prevalence of Menstrual Cycle Disorders in Female Athletes from Different Sports Disciplines: A Rapid Review. Int J. Environ. Res Public Health 19, 14243 (2022).
Paludo, A. C., Paravlic, A., Dvořáková, K. & Gimunová, M. The Effect of Menstrual Cycle on Perceptual Responses in Athletes: A Systematic Review With Meta-Analysis. Front Psychol. 13, 926854 (2022).
Winnard, A. et al. Systematic review of countermeasures to minimise physiological changes and risk of injury to the lumbopelvic area following long-term microgravity. Musculoskelet. Sci. Pr. 27, S5–S14 (2017).
Acknowledgements
This project was supported by the Rector’s Group for Space Research and Astronautics at Masaryk University, Brno, Czech Republic.
Author information
Authors and Affiliations
Contributions
M.G. and J.B.V.: conceptualization and search. A.C.P. and M.G.: data selection. M.B. and M.G.: data analysis. M.G., J.B.V., and A.C.P.: drafted manuscript. All authors critically revised the manuscript, contributed to the article, and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gimunová, M., Paludo, A.C., Bernaciková, M. et al. The effect of space travel on human reproductive health: a systematic review. npj Microgravity 10, 10 (2024). https://doi.org/10.1038/s41526-024-00351-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41526-024-00351-1