Abstract
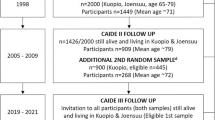
The Beijing Healthy Aging Cohort Study (BHACS) was established to supplement the limited data of a large representative cohort of older people based on the general population and was designed to evaluate the prevalence, incidence, and natural history of cognitive decline, functional disability, and conventional vascular risk factors. The aim was to determine the evolution of these conditions by estimating the rates and determinants of progression and regression to adverse outcomes, including dementia, cardiovascular events, cancer, and all-cause death. It can therefore provide evidence to help policy makers develop better policies to promote healthy aging in China. BHACS consisted of three cohorts (BLSA, CCHS-Beijing, and BECHCS) in Beijing with a total population of 11 235 (6281 in urban and 4954 in rural areas) and an age range of 55 years or older (55–101 years) with a mean age of 70.35 ± 7.71 years (70.69 ± 7.62 years in urban and 69.92 ± 7.80 years in rural areas). BHACS-BLSA conducted the baseline survey in 2009 with a multistage stratification-random clustering procedure for people aged 55 years or older; BHACS-CCHS-Beijing conducted the baseline survey in 2013–2015 with a stratified multistage cluster random sampling method for people aged 55 years or older; and BHACS-BECHCS conducted the baseline survey in 2010–2014 with two-stage cluster random sampling method for people aged 60 years or older. Data were collected through questionnaires, physical measurements, and laboratory analyses. Topics covered by BHACS include a wide range of physical and mental health indicators, lifestyles and personal, family, and socio-economic determinants of health. There are no immediate plans to make the cohort data freely available to the public, but specific proposals for further collaboration are welcome. For further information and collaboration, please contact the corresponding author Yao He (e-mail: yhe301@x263.net).


Similar content being viewed by others
References
Department of Economic and Social Affairs. The aging of population and its economic and social implications. United Nations; 1956. https://unog.primo.exlibrisgroup.com/permalink/41UNOG_INST/146850g/alma991001553369602391. Accessed 18 Oct 2022.
Department of Economic and Social Affairs. World Population prospects 2022: Summary of results. United Nations; 2022. https://doi.org/10.18356/9789210014380. Accessed 18 Oct 2022.
China Statistics Press. China Statistical Yearbook 2021. National Bureau of Statistics of China. 2022. http://www.stats.gov.cn/sj/ndsj/2021/indexch.htm. Accessed 22 Oct 2022.
Jiang Q, Feng Q, Editorial. Aging and health in China. Front Public Health. 2022;10:998769. https://doi.org/10.3389/fpubh.2022.998769.
Department of Ageing Health, National Aging Development Bulletin. National Health Commission of the People’s Republic of China. 2020; 2021. Accessed 22 Oct 2022. http://www.nhc.gov.cn/lljks/pqt/202110/c794a6b1a2084964a7ef45f69bef5423.shtml.
Fang EF, Xie C, Schenkel JA, et al. A research agenda for ageing in China in the 21st century (2nd edition): focusing on basic and translational research, long-term care, policy and social networks. Ageing Res Rev. 2020;64:101174. https://doi.org/10.1016/j.arr.2020.101174.
Zhang G, Yu C, Zhou M, Wang L, Zhang Y, Luo L. Burden of ischaemic heart disease and attributable risk factors in China from 1990 to 2015: findings from the global burden of disease 2015 study. BMC Cardiovasc Disord. 2018;18(1):18. https://doi.org/10.1186/s12872-018-0761-0.
Lopez-Otin C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Cell. 2013;153(6):1194–217. https://doi.org/10.1016/j.cell.2013.05.039.
Wang W, Liu Y, Liu J, et al. Mortality and years of life lost of cardiovascular diseases in China, 2005–2020: empirical evidence from national mortality surveillance system. Int J Cardiol. 2021;340:105–12. https://doi.org/10.1016/j.ijcard.2021.08.034.
Lautrup S, Sinclair DA, Mattson MP, Fang EF. NAD(+) in Brain Aging and Neurodegenerative Disorders. Cell Metab. 2019;30(4):630–55. https://doi.org/10.1016/j.cmet.2019.09.001.
Prince MJ, Wu F, Guo Y, et al. The burden of disease in older people and implications for health policy and practice. The Lancet. 2015;385(9967):549–62. https://doi.org/10.1016/s0140-6736(14)61347-7.
Cheng X, Yang Y, Schwebel DC, et al. Population ageing and mortality during 1990–2017: a global decomposition analysis. PLoS Med. 2020;17(6):e1003138. https://doi.org/10.1371/journal.pmed.1003138.
Pilleron S, Sarfati D, Janssen-Heijnen M, et al. Global cancer incidence in older adults, 2012 and 2035: a population-based study. Int J Cancer. 2019;144(1):49–58. https://doi.org/10.1002/ijc.31664.
Xu J, Wang J, Wimo A, Fratiglioni L, Qiu C. The economic burden of dementia in China, 1990–2030: implications for health policy. Bull World Health Organ. 2017;95(1):18–26. https://doi.org/10.2471/BLT.15.167726.
GBD 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the global burden of Disease Study 2019. The Lancet Public Health. 2022;7(2):e105–e25. https://doi.org/10.1016/s2468-2667(21)00249-8.
Dovjak P. Polypharmacy in elderly people. Wien Med Wochenschr. 2022;172(5–6):109–13. https://doi.org/10.1007/s10354-021-00903-0.
de Lima JD, Teixeira IA, Silva FO, Deslandes AC. The comorbidity conditions and polypharmacy in elderly patients with mental illness in a middle income country: a cross-sectional study. IBRO Rep. 2020;9:96–101. https://doi.org/10.1016/j.ibror.2020.07.008.
Park M, Reynolds CF. Depression among older adults with diabetes Mellitus. Clin Geriatr Med. 2015;31(1):117–37. https://doi.org/10.1016/j.cger.2014.08.022.
Gorska-Ciebiada M, Saryusz-Wolska M, Ciebiada M, Loba J. Mild cognitive impairment and depressive symptoms in elderly patients with diabetes: prevalence, risk factors, and comorbidity. J Diabetes Res. 2014;2014:179648. https://doi.org/10.1155/2014/179648.
Fan ZY, Yang Y, Zhang CH, Yin RY, Tang L, Zhang F. Prevalence and patterns of Comorbidity among Middle-Aged and Elderly People in China: a cross-sectional study based on CHARLS Data. Int J Gen Med. 2021;14:1449–55. https://doi.org/10.2147/IJGM.S309783.
Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13(1):57–65. https://doi.org/10.1517/14740338.2013.827660.
Komiya H, Umegaki H, Asai A, et al. Factors associated with polypharmacy in elderly home-care patients. Geriatr Gerontol Int. 2018;18(1):33–41. https://doi.org/10.1111/ggi.13132.
Enlund. JJ, Korhonen H, MJ, Sulkava. R, Hartikainen S. Patterns of drug use and factors associated with polypharmacy and excessive polypharmacy in elderly persons: results of the Kuopio 75 study: a cross-sectional analysis. Drugs Aging. 2009;26(6):493–503.
Tao L, Qu X, Gao H, Zhai J, Zhang Y, Song Y. Polypharmacy and potentially inappropriate medications among elderly patients in the geriatric department at a single-center in China: a retrospective cross-sectional study. Med (Baltim). 2021;100(42):e27494. https://doi.org/10.1097/MD.0000000000027494.
Roderka MN, Puri S, Batsis JA. Addressing obesity to promote healthy aging. Clin Geriatr Med. 2020;36(4):631–43. https://doi.org/10.1016/j.cger.2020.06.006.
Himes CL, Reynolds SL. Effect of obesity on falls, injury, and disability. J Am Geriatr Soc. 2012;60(1):124–9. https://doi.org/10.1111/j.1532-5415.2011.03767.x.
Kritchevsky SB, Beavers KM, Miller ME, et al. Intentional weight loss and all-cause mortality: a meta-analysis of randomized clinical trials. PLoS ONE. 2015;10(3):e0121993. https://doi.org/10.1371/journal.pone.0121993.
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82. https://doi.org/10.1001/jama.2012.113905.
Martinez-Tapia C, Diot T, Oubaya N et al. The obesity paradox for mid- and long-term mortality in older cancer patients: a prospective multicenter cohort study. Am J Clin Nutr. 2020;nqaa238.
Bijani A, Cumming RG, Hosseini SR, et al. Obesity paradox on the survival of elderly patients with diabetes: an AHAP-based study. J Diabetes Metab Disord. 2018;17(1):45–51. https://doi.org/10.1007/s40200-018-0337-7.
Keating N. A research framework for the United Nations Decade of healthy ageing (2021–2030). Eur J Ageing. 2022;19(3):775–87. https://doi.org/10.1007/s10433-021-00679-7.
Rudnicka E, Napierala P, Podfigurna A, Meczekalski B, Smolarczyk R, Grymowicz M. The World Health Organization (WHO) approach to healthy ageing. Maturitas. 2020;139:6–11. https://doi.org/10.1016/j.maturitas.2020.05.018.
Global Report. World report on Ageing and Health. World Health Organization. 2015. https://www.who.int/publications/i/item/9789241565042. Accessed 26 Sep 2022.
Hu D, Yan W, Zhu J, Zhu Y, Chen J. Age-related Disease Burden in China, 1997–2017: findings from the global burden of Disease Study. Front Public Health. 2021;9:638704. https://doi.org/10.3389/fpubh.2021.638704.
World Health Assembly 50. The World health report 1997: conquering suffering, enriching humanity: summary. World Health Organization. 1997. https://apps.who.int/iris/handle/10665/179593. Accessed 26 Sep 2022.
Nie P, Li Y, Zhang N, Sun X, Xin B, Wang Y. The change and correlates of healthy ageing among chinese older adults: findings from the China health and retirement longitudinal study. BMC Geriatr. 2021;21(1):78. https://doi.org/10.1186/s12877-021-02026-y.
Zhang Q, Wu Y, Han T, Liu E. Changes in cognitive function and risk factors for cognitive impairment of the Elderly in China: 2005–2014. Int J Environ Res Public Health. 2019;16(16):2847. https://doi.org/10.3390/ijerph16162847.
Yang Y, Meng Y. Is China moving toward healthy aging? A Tracking Study based on 5 phases of CLHLS Data. Int J Environ Res Public Health. 2020;17(12):4343. https://doi.org/10.3390/ijerph17124343.
Zhang T, Liu C, Lu B, Wang X. Changes of inequality in functional disability of older populations in China from 2008 to 2018: a decomposition analysis. BMC Geriatr. 2022;22(1):308. https://doi.org/10.1186/s12877-022-02987-8.
Zhou YF, Song XY, Wu J, et al. Association between dietary patterns in midlife and healthy ageing in chinese adults: the Singapore Chinese Health Study. J Am Med Dir Assoc. 2021;22(6):1279–86. https://doi.org/10.1016/j.jamda.2020.09.045.
Guo Y, Ge T, Mei L, Wang L, Li J. Widowhood and Health Status among Chinese older adults: the Mediation Effects of different types of support. Front Public Health. 2021;9:745073. https://doi.org/10.3389/fpubh.2021.745073.
Jiang J, Tang Z, Futatsuka M. The impact of ADL disability on depression symptoms in a community of Beijing elderly, China. Environ Health Prev Med. 2002;7(5):199–204. https://doi.org/10.1007/BF02898005.
Tang Z, Wang HX, Meng C, et al. The prevalence of functional disability in activities of daily living and instrumental activities of daily living among elderly Beijing Chinese. Arch Gerontol Geriatr. 1999;29(2):115–25. https://doi.org/10.1016/s0167-4943(99)00026-6.
Fang X, Wang Z, Wang C, et al. Cardiovascular and Cognitive Health Study in Middle-Aged and Elderly residents of Beijing(CCHS-Beijing): design and rationale. Neuroepidemiology. 2016;46(3):182–90. https://doi.org/10.1159/000443707.
Acknowledgements
All authors thank the Beijing Longitudinal Study of Aging team, the Cardiovascular and Cognitive Health Study in Middle-Aged and Elderly Residents of Beijing team, and the Beijing Elderly Comprehensive Health Cohort Study team for providing data and sharing the use of the data sets in the Beijing Healthy Aging Cohort Study. We thank all volunteers and staff involved in this research.
Funding
This work was supported by the National Natural Science Foundation of China (82173589, 82173590); Capital’s Funds for Health Improvement and Research (2022-2G-5031); National Key Research and Development Program of China (2022YFC2503605); the National Key Program in the Twelfth Five-year Plan (Grant No. 2011BAI 11 B01) from the Chinese Ministry of Science and Technology; Commission of Science and Technology of Beijing (Grant No. D121100004912002); and Beijing Municipal Science & Technology Commission (Z171100001017019).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Xianghua Fang, Yao He, Zhe Tang, and Miao Liu designed the Study. Yao He, Miao Liu, Chunxiu Wang, Shanshan Yang, Jianhua Wang, Chengbei Hou, Shengshu Wang, Xiaoying Li, and Hongbing Yang directed the study’s implementation. Junhan Yang, Haowei Li, Shaohua Liu, Yang Song, Shimin Chen, Shimin Hu, Xuehang Li, Zhiqiang Li, Rongrong Li, Huaihao Li, Yinghui Bao, and Yueting Shi designed the analytical strategy and helped to interpret the findings. Junhan Yang, Huaihao Li, Yinghui Bao, and Yueting Shi helped to write the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
BHACS was performed in line with the principles of the Declaration of Helsinki, approved by the Ethics Committee of Chinese PLA General Hospital (S2022-412-02), and registered by the China Clinical Trial Registry (ChiCTR2200066177).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, M., Yang, J., Wang, C. et al. Cohort profile: Beijing Healthy Aging Cohort Study (BHACS). Eur J Epidemiol 39, 101–110 (2024). https://doi.org/10.1007/s10654-023-01050-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-023-01050-z