Abstract
Background
Several studies have been conducted to understand the impact of socioeconomic and maternal factors on child undernutrition. However, the past literature has not directly examined the joint impacts of fuel use and ambient pollution and have primarily focused on PM2.5.
Objective
This study explored the individual and community-level associations of both indoor (cooking fuel type) and ambient air pollution (PM2.5, NO2 and SO2) during maternal gestation on child undernutrition.
Methods
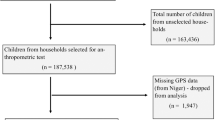
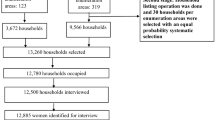
This study analysed stunting, being underweight, and anaemia of children aged 0–59 months (n = 259,627) using the National Family Health Survey. In-utero exposures to ambient PM2.5, NO2, and SO2 were measured using satellite data and self-reported fuel type was a marker of indoor pollution exposure. The study used univariate and bivariate Moran’s I, spatial lag model and multivariable logistic regression models after adjusting for other covariates to understand the effect of pollution on in-utero exposure and child health status at the individual and community-levels.
Results
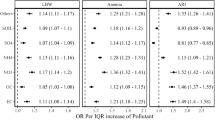
Higher concentration of indoor and ambient air pollution was found in the Northern and parts of Central regions of India. Estimates of spatial modelling show that each 1 μg/m–3 increase in maternal exposure to ambient PM2.5 across the clusters of India was associated with a 0.11, 9 and 19 percentage points increase in the prevalence of stunting, underweight and anaemia, respectively. The results of multi-pollutant model show that a higher ambient PM2.5 exposure during pregnancy was linked to higher odds of stunting (AOR:1.38; 95% CI:1.32–1.44), underweight (AOR:1.59; 95% CI:1.51–1.67) and anaemia (AOR:1.61; 95% CI:1.52–1.69) in children. Weaker but similar associations were observed for NO2, but not with SO2. Indoor pollution exposure during in-utero periods was also significantly associated with childhood undernutrition and this association was modified by ambient PM2.5 levels, where exposure to both indoor and ambient air pollution had even greater odds of being undernourished.
Impact statement
-
Our research on multi-pollutant models has revealed the initial proof of the individual impacts of indoor and outdoor pollution (PM2.5, NO2, and SO2) exposure during fetal development on children’s nutrition.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The study uses secondary data which are available on reasonable request through https://dhsprogram.com/data/ and https://giovanni.gsfc.nasa.gov/giovanni/. The data and code used in this study are available from the corresponding author on reasonable request.
References
Keeley B, Little C. The State of the Worlds Children 2017: Children in a Digital World, UNICEF, Dec. 2017. Accessed: Nov. 29, 2022. [Online]. https://eric.ed.gov/?id=ED590013.
Cusick SE, Georgieff MK. The Role of Nutrition in Brain Development: The Golden Opportunity of the ‘First 1000 Days. J Pediatr. 2016;175:16–21. https://doi.org/10.1016/j.jpeds.2016.05.013.
Bourke CD, Berkley JA, Prendergast AJ. Immune Dysfunction as a Cause and Consequence of Malnutrition. Trends Immunol. 2016;37:386–98. https://doi.org/10.1016/j.it.2016.04.003.
Liu J, Raine A, Venables PH, Dalais C, Mednick SA. Malnutrition at Age 3 Years and Lower Cognitive Ability at Age 11 Years: Independence From Psychosocial Adversity. Arch Pediatr Adolesc Med. 2003;157:593–600. https://doi.org/10.1001/archpedi.157.6.593.
Tomkins A. Malnutrition, morbidity and mortality in children and their mothers. Proc Nutr Soc. 2000;59:135–46. https://doi.org/10.1017/s0029665100000161.
Martins VJB, Florêncio TMMT, Grillo LP, Franco MDCP, Martins PA, Clemente APG, et al. Long-Lasting Effects of Undernutrition. Int J Environ Res Public Health. 2011;8:1817–46. https://doi.org/10.3390/ijerph8061817.
Hoddinott J, Maluccio JA, Behrman JR, Flores R, Martorell R. Effect of a nutrition intervention during early childhood on economic productivity in Guatemalan adults. Lancet. 2008;371:411–6. https://doi.org/10.1016/S0140-6736(08)60205-6.
Victora CG, Christian P, Vidaletti LP, Gatica-Domínguez G, Menon P, Black RE. Revisiting maternal and child undernutrition in low-income and middle-income countries: variable progress towards an unfinished agenda. Lancet. 2021;397:1388–99. https://doi.org/10.1016/S0140-6736(21)00394-9.
Dey D, Jana A, Pradhan MR. Influence of agriculture on child nutrition through child feeding practices in India: A district-level analysis. PLoS ONE. 2021;16:e0261237 https://doi.org/10.1371/journal.pone.0261237.
Sinha RK, Dua R, Bijalwan V, Rohatgi S, Kumar P. Determinants of Stunting, Wasting, and Underweight in Five High-Burden Pockets of Four Indian States. Indian J Commun Med. 2018;43:279–83. https://doi.org/10.4103/ijcm.IJCM_151_18.
Wali N, Agho K, Renzaho AMN. Past drivers of and priorities for child undernutrition in South Asia: a mixed methods systematic review protocol. Syst Rev. 2019;8:189 https://doi.org/10.1186/s13643-019-1112-7.
IIPS and ICF, National Family Healh Survey, international Institute for Population Sciences, Mumbai, 2022, [Online]. http://rchiips.org/nfhs/NFHS-5Reports/NFHS-5_INDIA_REPORT.pdf.
Luby SP, Rahaman M, Arnold BF, Unicomb L, Ashraf S, Winch PJ, et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Bangladesh: a cluster randomised controlled trial. Lancet Glob Health. 2018;6:e302–15. https://doi.org/10.1016/S2214-109X(17)30490-4.
Shah PS, Balkhair T. Air pollution and birth outcomes: a systematic review. Environ Int. 2011;37:498–516. https://doi.org/10.1016/j.envint.2010.10.009.
Malmqvist E, Rignell-Hydbom A, Tinnerberg H, Bjork J, Stroh E, Jakobsson, et al. Maternal exposure to air pollution and birth outcomes. Environ Health Perspect. 2011;119:553–8. https://doi.org/10.1289/ehp.1002564.
Borlaza LJS, Uzu G, Ouidir M, Lyon-Caen S, Marsal A, Weber S, et al. Personal exposure to PM2.5 oxidative potential and its association to birth outcomes. J Expo Sci Environ Epidemiol. 2022:1–11. https://doi.org/10.1038/s41370-022-00487-w.
Trasande L, Wong K, Roy A, Savitz DA, Thurston G. Exploring prenatal outdoor air pollution, birth outcomes and neonatal health care utilization in a nationally representative sample. J Expo Sci Environ Epidemiol. 2013;23:Art.3 https://doi.org/10.1038/jes.2012.124.
Larson PS, Espira L, Glenn BE, Larson MC, Crowe CS, Jang S, et al. Long-Term PM2.5 Exposure Is Associated with Symptoms of Acute Respiratory Infections among Children under Five Years of Age in Kenya, 2014. Int J Environ Res Public Health. 2022;19:2525 https://doi.org/10.3390/ijerph19052525.
Chillrud SN, Ae-Ngibise KA, Gould CF, Owusu-Agyei S, Mujtaba M, Manu G, et al. The effect of clean cooking interventions on mother and child personal exposure to air pollution: results from the Ghana Randomized Air Pollution and Health Study (GRAPHS). J Expo Sci Environ Epidemiol. 31, Art. Jul. 2021, https://doi.org/10.1038/s41370-021-00309-5.
Wendling ZA, Emerson JW, de Sherbinin A, Esty DC. Environmental Performance Index 2020—Global Metrics for the Environment: Ranking Country Performance on Sustainability Issues. Yale Center for Environmental Law & Policy: New Haven, CT, USA. 2020.
Swaminathan S, Hemalatha R, pandey A, Kassenbaum NJ, Lamiah A, Longvah T, et al. The burden of child and maternal malnutrition and trends in its indicators in the states of India: the Global Burden of Disease Study 1990–2017. Lancet Child Adolesc Health. 2019;3:855–70. https://doi.org/10.1016/S2352-4642(19)30273-1.
Bali Sagnik Dey PS, Chowdhury S, and Kunal, Early life exposure to outdoor air pollution: Effect on child health in India, Brookings, Mar. 12, 2019. https://www.brookings.edu/research/early-life-exposure-to-outdoor-air-pollution-effect-on-child-health-in-india/ (accessed May 21, 2022).
Spears D, Dey S, Chowdhury S, Scovronick N, Vyas S, Apte J. The association of early-life exposure to ambient PM2.5 and later-childhood height-for-age in India: an observational study. Environ Health. 2019;18:62 https://doi.org/10.1186/s12940-019-0501-7.
Goddard Earth Sciences Data and Information Services Center (GES DISC), Global Modeling and Assimilation Office (GMAO)(2015), MERRA-2 tavg1_2d_slv_Nx: 2d, 1-Hourly, Time-Averaged, Single-Level, Assimilation, Single-Level Diagnostics V5. 12.4. NASA, 2015. [Online]. https://doi.org/10.5067/VJAFPLI1CSIV.
W. M. G. R. S. Group, de Onis M. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr. 2006;95:76–85. https://doi.org/10.1111/j.1651-2227.2006.tb02378.x.
Hamed E, Syed MA, Alemrayat BF, Tirmizi SHA, Alnuaimi AS. Haemoglobin cut-off values for the diagnosis of anaemia in preschool-age children. Am J Blood Res. 2021;11:248–54.
Mehta U, Dey S, Chowdhury S, Ghosh S, Hart JE, Kurpad A. The Association Between Ambient PM2.5 Exposure and Anemia Outcomes Among Children Under Five Years of Age in India. Environ Epidemiol. 2021;5:e125 https://doi.org/10.1097/EE9.0000000000000125.
Singh N, Murari V, Kumar M, Barman SC, Banerjee T. Fine particulates over South Asia: Review and meta-analysis of PM2.5 source apportionment through receptor model. Environ Pollut. 2017;223:121–36. https://doi.org/10.1016/j.envpol.2016.12.071.
Brauer M, brook JR, Christidis T, chu Y, Crouse DL, Erickson A, et al. Mortality–Air Pollution Associations in Low-Exposure Environments (MAPLE): Phase 2. Res Rep Health Eff Inst. 2022;2022:203.
Guo H, Kota SH, Sahu SK, Hu J, Ying Q, Gao A, et al. Source apportionment of PM2.5 in North India using source-oriented air quality models. Environ Pollut. 2017;231:426–36. https://doi.org/10.1016/j.envpol.2017.08.016.
Sahu SK, Mangaraj P, Beig G, Samal A, Pradhan C, Dash S, et al. Quantifying the high resolution seasonal emission of air pollutants from crop residue burning in India. Environ Pollut. 2021;286:117165 https://doi.org/10.1016/j.envpol.2021.117165.
Chowdhury S, Dey S, Guttikunda S, Pillarisetti A, Smith KR, Girolamo LD. Indian annual ambient air quality standard is achievable by completely mitigating emissions from household sources. PNAS. 2019;116:10711–6. https://doi.org/10.1073/pnas.1900888116.
Bhanarkar AD, Purohit P, Rafaj P, Amann M, Bertok I, Cofala J, et al. Managing future air quality in megacities: Co-benefit assessment for Delhi. Atmos Environ. 2018;186:158–77. https://doi.org/10.1016/j.atmosenv.2018.05.026.
Singh GK, Choudhary V, Rajeev P, Paul D, Gupta T. Understanding the origin of carbonaceous aerosols during periods of extensive biomass burning in northern India. Environ Pollut. 2021;270:116082 https://doi.org/10.1016/j.envpol.2020.116082.
Guttikunda SK, Jawahar P. Atmospheric emissions and pollution from the coal-fired thermal power plants in India. Atmos Environ. 2014;92:449–60. https://doi.org/10.1016/j.atmosenv.2014.04.057.
Ramachandran A, Jain NK, Sharma SA, Pallipad J. Recent trends in tropospheric NO2 over India observed by SCIAMACHY: Identification of hot spots. Atmos Pollut Res. 2013;4:354–61. https://doi.org/10.5094/APR.2013.040.
Prasad AK, Singh RP, Kafatos M. Influence of coal-based thermal power plants on the spatial–temporal variability of tropospheric NO2column over India. Environ Monit Assess. 2012;184:1891–907. https://doi.org/10.1007/s10661-011-2087-6.
Balietti A, Datta S, and Veljanoska S, Air pollution and child development in India, HAL, Post-Print, 2022. Accessed: May 21, 2022. [Online]. https://econpapers.repec.org/paper/haljournl/hal-03662124.htm.
Li X, Huang S, Jiao A, Yang X, Yun J, Wang Y, et al. Association between ambient fine particulate matter and preterm birth or term low birth weight: An updated systematic review and meta-analysis. Environ Pollut. 2017;227:596–605. https://doi.org/10.1016/j.envpol.2017.03.055.
Prendergast AJ, Humphrey JH. The stunting syndrome in developing countries. Paediatr Int Child Health. 2014;34:250–65. https://doi.org/10.1179/2046905514Y.0000000158.
Ram PK, Dutt D, Silk BJ, Doshi S, Rudra CB, Abedin J, et al. Household Air Quality Risk Factors Associated with Childhood Pneumonia in Urban Dhaka, Bangladesh. Am J Trop Med Hyg. 2014;90:968–75. https://doi.org/10.4269/ajtmh.13-0532.
Guensch DP, Michel MC, Huttenmoser SP, Jung B, Gulac P, Segiser A. et al. The blood oxygen level dependent (BOLD) effect of in-vitro myoglobin and hemoglobin. Sci Rep. 11, Art. Jun. 2021, https://doi.org/10.1038/s41598-021-90908-x.
Tian Y, Li Y, Sun S, Dong Y, Tian Z, Zhan L, et al. Effects of urban particulate matter on the quality of erythrocytes. Chemosphere. 2023;313:137560 https://doi.org/10.1016/j.chemosphere.2022.137560.
Mesdaghinia A, Pourpak Z, Naddafi K, Nodehi RN, Alizadeh Z, Rezaei S, et al. An in vitro method to evaluate hemolysis of human red blood cells (RBCs) treated by airborne particulate matter (PM10). MethodsX. 2019;6:156–61. https://doi.org/10.1016/j.mex.2019.01.001.
Torres-Ramos YD, Montoya-Estrada A, Guzman-Grenfell AM, Mancilla-Ramirez J, Cardenas-Gonzalez B, Blanco-Jimenez S, et al. Urban PM2.5 induces ROS generation and RBC damage in COPD patients. Front Biosci (Elite Ed). 2011;3:808–17. https://doi.org/10.2741/e288.
Elbarbary M, Honda T, Morgan G, Guo Y, guo Y, kowal P, et al. Ambient Air Pollution Exposure Association with Anaemia Prevalence and Haemoglobin Levels in Chinese Older Adults. Int J Environ Res Public Health. 17, Art. Jan. 2020, https://doi.org/10.3390/ijerph17093209.
Bárány P. Inflammation, serum C‐reactive protein, and erythropoietin resistance. Nephrol Dialysis Transplant. 2001;16:224–7. https://doi.org/10.1093/ndt/16.2.224.
Viehmann A, Hertel S, Fuks K, Eisele L, Moebus S, Mohlenkamp S, et al. Long-term residential exposure to urban air pollution, and repeated measures of systemic blood markers of inflammation and coagulation. Occup Environ Med. 2015;72:656–63. https://doi.org/10.1136/oemed-2014-102800.
Srám RJ, Binková B, Dejmek J, Bobak M. Ambient air pollution and pregnancy outcomes: a review of the literature. Environ Health Perspect. 2005;113:375–82. https://doi.org/10.1289/ehp.6362.
Ritz B, Wilhelm M. Ambient Air Pollution and Adverse Birth Outcomes: Methodologic Issues in an Emerging Field. Basic Clin Pharm Toxicol. 2008;102:182–90. https://doi.org/10.1111/j.1742-7843.2007.00161.x.
Burris HH, Baccarelli AA. Air pollution and in utero programming of poor fetal growth. Epigenomics. 2017;9:213–6. https://doi.org/10.2217/epi-2017-0008.
Rider CF, Carlsten C. Air pollution and DNA methylation: effects of exposure in humans. Clin Epigenet. 2019;11:131 https://doi.org/10.1186/s13148-019-0713-2.
Ehsanifar M, Jafari AJ, Nikzad H, Zavareh MS, Atlasi MA, Mohammadi H, et al. Prenatal exposure to diesel exhaust particles causes anxiety, spatial memory disorders with alters expression of hippocampal pro-inflammatory cytokines and NMDA receptor subunits in adult male mice offspring. Ecotoxicol Environ Saf. 2019;176:34–41. https://doi.org/10.1016/j.ecoenv.2019.03.090.
Datt G, Maitra P, Menon N, Ray R. Coal Plants, Air Pollution and Anaemia: Evidence from India. The Journal of development studies. 2023;59:533–51.
Rahman MS, Howlader T, Masud MS, Rahman ML. Association of Low-Birth Weight with Malnutrition in Children under Five Years in Bangladesh: Do Mother’s Education, Socio-Economic Status, and Birth Interval Matter? PLOS ONE. 2016;11:e0157814 https://doi.org/10.1371/journal.pone.0157814.
Kankaria A, Nongkynrih B, Gupta SK. Indoor Air Pollution in India: Implications on Health and its Control. Indian J Community Med. 2014;39:203–7. https://doi.org/10.4103/0970-0218.143019.
Smith KR, McCracken JP, Weber MW, Hubbard A, Jenny A, Thompson LM, et al. Effect of reduction in household air pollution on childhood pneumonia in Guatemala (RESPIRE): a randomised controlled trial. Lancet. 2011;378:1717–26. https://doi.org/10.1016/S0140-6736(11)60921-5.
Jana A, Varghese JS, Naik G. Household air pollution and cognitive health among Indian older adults: Evidence from LASI. Environ Res. 2022;214:113880 https://doi.org/10.1016/j.envres.2022.113880.
Upadhyay AK, Singh A, Kumar K, Singh A. Impact of indoor air pollution from the use of solid fuels on the incidence of life threatening respiratory illnesses in children in India. BMC Public Health. 2015;15:300 https://doi.org/10.1186/s12889-015-1631-7.
Islam S, Rana MJ, Mohanty SK. Cooking, smoking, and stunting: Effects of household air pollution sources on childhood growth in India. Indoor Air. 2021;31:229–49. https://doi.org/10.1111/ina.12730.
Acknowledgements
The authors acknowledge the Ministry of Health and Family Welfare (MoHFW), Government of India for funding and providing the National Family Health Survey (NFHS) (http://rchiips.org/nfhs/). We gratefully acknowledge the University Grants Commission (UGC) for the doctoral fellowship received by Arup Jana and Akancha Singh for the research work. The authors express their gratitude to NASA for making the data on air pollution available in the public domain.
Author information
Authors and Affiliations
Contributions
Conceptualisation: AJ, AC. Data curation: AJ. Formal analysis: AJ. Methodology: AJ, AC. Software: AJ. Writing: AJ, AC, AS. Review & editing: AC, AS, AJ, SDA, JD.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The organization committee of the survey received ethical approval from the Ministry of Health and Family Welfare (MoHFW) to collect the human data. The Indian Demographic and Health Survey (DHS) is known as National Family Health Survey (NFHS) in India. We used published large-scale national data where every respondent was anonymized in the data set itself. As it is not based on a primary survey- cases, we were not required to do any anonymization in the study as the data is already made in that fashion following all ethical protocols. Thereby, it is certified that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of the survey. Also, verbal as well as written informed consent was obtained from all the participants. The informed consent was taken from their parent or legal guardian. The dataset is publicly available, thus, consent for publication is not applicable for the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jana, A., Singh, A., Adar, S.D. et al. In-utero exposure to multiple air pollutants and childhood undernutrition in India. J Expo Sci Environ Epidemiol (2023). https://doi.org/10.1038/s41370-023-00591-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41370-023-00591-5