Abstract
Background
Although ~18 million people live within a mile from active oil and gas development (OGD) sites in the United States, epidemiological research on how OGD affects the health of nearby urban residents is sparse. Thousands of OGD sites are spread across Los Angeles (LA) County, California, home to the largest urban oil production in the country. Air pollution and noise from OGD may contribute to cardiovascular morbidity.
Objective
We examined the association between proximity to OGD and blood pressure in a diverse cohort of residents in LA.
Methods
We recruited residents in South LA who lived <1 km from an OGD site. We collected three blood pressure measurements for each participant and used the second and third measurements to calculate averages for systolic blood pressure (SBP) and diastolic blood pressure (DBP) separately. We conducted multivariable linear regression to examine the relationship between distance to OGD sites and continuous SBP and DBP, adjusting for BMI, smoking status, distance to freeway, sex, age, and use of antihypertension medications, with a random effect for household. We examined effect measure modification by BMI category and smoking category.
Results
Among the 623 adult participants, we found that for every 100 meter increase in distance from the OGD site, DBP was reduced by an average of 0.73 mmHg (95% CI: −1.26, −0.21) in this population. We observed stronger effects of proximity to OGD site on DBP among never smokers and among participants with a healthy BMI. The associations observed between proximity to OGD site and SBP were weaker but followed the same patterns as those for DBP.
Impact
Our study suggests that living near urban oil drilling sites is significantly associated with greater diastolic blood pressure in urban Los Angeles communities. This research improves understanding of impacts from living nearby drilling operations on the health and welfare of this community, which is critical to inform public health relevant strategies.
Similar content being viewed by others
Introduction
In response to a drive for energy independence coupled with demands for fossil fuels, domestic oil and gas production in the United States (US) has surged over the last decade [1]. Across the continental US, there are over 1 million onshore oil and gas wells with an estimated 18 million people living <1600 m from an active oil extraction site in the US [2]. Increasingly, petroleum extraction is occurring in densely populated areas, and yet, epidemiological research on the health consequences for nearby urban residents is sparse [3,4,5,6]. California (CA), together with Texas, North Dakota, and Alaska account for ~60% of all oil produced domestically. Public health concern has accompanied this rapid growth in oil production [7].
Los Angeles (LA) County, CA, is home to one of the most petroleum-dense basins in the world, with thousands of extraction wells spread across multiple oil fields in 70 different communities [8, 9]. Land development, population growth, and oil exploration in LA occurred concurrently, leaving a patchwork of thousands of oil wells operating in very close proximity to homes, schools and parks [10]. Approximately 1/3rd of the 10 million LA County residents live less than 1 mile from an active oil or gas extraction site, and over 500,000 residents live less than 400 m away [10]. A single well typically operates for decades with neighbors facing impacts from construction, production, processing and transportation. Chemicals associated with oil extraction and production include carcinogens, mutagens, reproductive toxins, irritants and endocrine disruptors [4, 11,12,13]. These compounds can enter the nearby environment through spills, leaks, volatilization, and disposal [4, 11,12,13,14]. Research in California has identified increase air pollution, adverse birth outcomes and decreased respiratory function within 1 km of well sites [15,16,17].
Recent research demonstrates multiple health-hazardous air pollutants associated with petroleum extraction, including particulate matter (PM), nitric oxides (NOx), and volatile organic compounds (VOCs) including polyaromatic hydrocarbons, benzene, naphthalene, xylenes, toluene, ethylbenzene and formaldehyde [18,19,20]. Exposure to environmental stressors generated by OGD, such as air pollution, noise, and psychosocial stress, have been shown to individually and jointly contribute to cardiovascular morbidity and mortality in other environmental contexts [21]. Prior research has shown that inhalation of air pollutants can result in several adverse cardiovascular responses, including elevations in blood pressure (BP) [22, 23]. Elevated blood pressure is a leading risk factor for the global burden of disease and is strongly and directly related to cardiovascular disease (CVD), which remains the leading cause of morbidity and mortality in the United States [24, 25]. Epidemiological studies have consistently found that PM2.5 ambient air pollution is associated with a small, yet significant, increase in blood pressure [26,27,28]. While less widely studied, there is evidence of an association between exposures to VOCs with cardiovascular mortality, cardiovascular disease, and higher blood pressure [29, 30].
Although OGD generates multiple exposures that have been consistently linked to cardiovascular health risks, few studies have examined OGD impacts on blood pressure on nearby residents. Epidemiological studies have observed a positive association between proximity to OGD and prevalence of cardiology inpatient hospital admission in rural Pennsylvania [31]. A cross-sectional study in rural Colorado measured higher blood pressure among adults living in areas with higher density of wells compared to those farther away [32]. In a diverse cohort of residents living near urban oil drilling in Los Angeles, we examined the association between proximity to OGD and blood pressure.
Methods
This study used a community-based participatory research approach to recruit from neighborhoods atop the Las Cienegas oilfield situated in South Los Angeles, CA as one component of the Health and Air Pollution Study [17]. These are densely populated neighborhoods of predominantly low-income Black and Latinx/Hispanic families facing disproportionate burden of environmental hazards [33, 34]. Participants were drawn from residents living <1 km from either (1) a well site with 28 wells that was actively producing oil during the entire study period; or (2) a site housing 21 wells which were idle (i.e., not actively producing any oil or gas) during the study period, but had previously been active for decades. To be eligible for the Health and Air Pollution study, participants were at least 9 years old, spoke English, Spanish or Korean, and lived within 1000 m of one of the oil sites of interest for at least 2 years. The research was a community-academic collaboration with local community health workers together with Esperanza Community Housing and Redeemer Community Partners, both community-based organizations working in the neighborhoods. Details on the recruitment methods are available elsewhere [17]. The study was approved by the University of Southern California Institutional Review Board. Participants who provided written consent completed a baseline demographic and health questionnaire and provided physiological measurements.
Health questionnaire
A questionnaire was administered in the participant’s preferred language (Spanish, English or Korean) and participants were asked sociodemographic information, race/ethnicity, sex, age, tobacco exposure (e.g., smoking history, current smoking practices, presence of indoor environmental tobacco smoke), occupation, medication use and residential history. We collected information about disease history, including if the participant ever had a doctor-diagnosis of hypertension. We reviewed the participant-reported medication usage and identified participants who were currently taking anti-hypertensive medications.
Cardiovascular health and physiological measurements
For each adult participant, we collected 3 blood pressure measurements using an Omron 705IT (Omron Corporation, Kyoto, Japan) [35] by trained study staff. To obtain these measures, an adjustable, inflatable cuff was fitted to a participant’s dominant arm, which was extended onto a flat surface, ensuring that the bend in the elbow was at heart level with feet flat on the floor. The participant rested 5 min before we collected three measurements, each 1 min apart. The reported systolic blood pressure (SBP) and diastolic blood pressure (DBP) is the average of the 2nd and 3rd measurements. Each participant’s height (to nearest 0.1 cm) and weight (0.1 kg) were measured and used to calculate and categorize participant body mass index (BMI, underweight: <18.5 healthy: 18.5–24.9, overweight: 25–29.9, obese: 30+, according to the categories from the National Heart, Lung, and Blood Institute). Due to the small number of underweight participants, these participants were combined with the healthy BMI category for analysis. The measurements were shared back with the participants at the end of the visit along with clinic guidelines to aid interpretation of the results.
Exposure metrics
The location and status of the wells was retrieved from the California Geologic Energy Management Division (CalGEM) for the study period. Participant addresses were geocoded and the Euclidean distance to the well sites and freeways was calculated. Daily PM2.5 concentrations were estimated for the day of the study visit based on the Los Angeles North Main Street monitor, located ~4–5 miles northeast from the study area and operated by South Coast Air Quality Management District.
Statistical analysis
We conducted exploratory data analysis, examining participant characteristics by hypertensive status (based on participant-reported doctor-diagnosed hypertension), proximity to OGD sites, and variable distributions. We found continuous SBP and DBP to approximate a normal distribution and proceeded with untransformed variables for subsequent analyses. We conducted multivariable linear regression to assess the relationship between distance to OGD sites and continuous SBP and DBP, adjusting for BMI category (healthy, overweight, obese), use of anti-hypertensive medications, smoking status (current, former, never), distance to freeway (<200 m from highway vs. ≥200 m from highway), sex, and age (continuous) [36]. As participants could live in the same household as other participants, we conducted all analyses with a random effect for household. We examined effect measure modification by BMI category, smoking category, and race/ethnicity.
Secondary analyses
Given that approximately one-fifth of participants (n = 129) reported taking anti-hypertensive medications, we further explored this relationship using adjusted blood pressure measurements for participants on anti-hypertensive medications by adding 15 mmHg to the SBP values and 10 mmHg to DBP values, based on methods from prior research [36,37,38]. We also conducted analyses where we excluded participants taking anti-hypertensive medication and participants who reported doctor-diagnosed hypertension. Because PM2.5 has been acutely associated with BP [26], we adjusted for PM2.5 daily average on the day BP was assessed. Finally, we examined the association between distance to OGD site and the presence of measured stage 1 hypertension, defined as SBP > 130 mmHg or DBP > 80 mmHg [39]. All analyses were conducted in R 4.1.0.
Results
A total of 665 adult residents (at least 18 years of age) participated in this neighborhood study to measure physical health symptoms from 488 distinct addresses [17]. Eleven participants were subsequently excluded for living outside of the study area after confirmation of residential address, 8 participants were excluded for outlier BP measurements (systolic BP > 180 mm Hg or diastolic BP > 120 mm Hg, which may reflect error in cuff size fitting or placement), and 16 participants did not complete BP measurements. Seven additional participants were excluded from analysis because of missing key covariates (sex and or height). This resulted in a total population of 623 individuals. The mean age of the participants was 49 years (range 18–85) with 22.6% of participants over the age of 65. The majority were female (66.8 %) and all participants identified as people of color (Black, Latinx/Hispanic, Asian or multi-racial) (Table 1). Forty-one percent of participants were considered obese, reflecting the general rates of obesity in South LA [40]. Eight percent were current smokers. On average, participants had lived in the neighborhood for 19 years. The median distance between the home and the OGD site was 260 meters (range: 39–970 m). The mean SBP and DBP measurements for the analysis cohort were 124.7 ± 18.6 and 79.5 ± 11.1 mmHg, respectively. Approximately 57% of the cohort met the criteria of state 1 hypertension (average measure >130 mmHg SBP or >80 mmHg DBP).
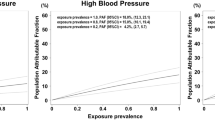
In multivariable linear models, we observed that greater distance from the oil and gas wells was associated with lower blood pressure, on average, when adjusting for BMI, smoking status, distance from freeway, sex, age and use of anti-hypertensive medication. This finding was statistically significant for DBP, showing that for every 100 m increase in residential distance from the OGD site, DBP was reduced by an average of 0.73 mmHg (95% CI: −1.26, −0.21) in this population (Fig. 1 and Table S1). The effect was smaller and not statistically significant for SBP, with a reduction by 0.24 mmHg (95% CI: −1.04, 0.55) per 100 m increase in distance. The results were consistent when including the outlier measurements (Table S2).
Association between systolic and diastolic blood pressure (mmHg) and distance from the OGD site (per 100 m) among all adult participants (adjusted for BMI, smoking status, distance from freeway, sex, age and use of anti-hypertensive medication, with a household random effect) and stratified by smoking status and BMI category.
We stratified the analysis considering two risk factors for elevated blood pressure: smoking status and BMI (Fig. 1). We observed stronger effects of distance on blood pressure among the never smokers, with an increase of 100 m in distance from the OGD site associated with, on average, a 0.48 mmHg (95% CI −1.40, 0.44) and 0.88 mmHg (95% CI −1.46, −0.30) decrease in SBP and DBP, respectively. Among the participants with a healthy BMI (BMI < 25 based on measured height and weight), we observed a reduction of 1.06 mmHg (95% CI −2.93, 0.81) and 1.77 mmHg (95% CI −2.89, −0.64) in SBP and DBP respectively for each 100 m increase in residential distance from the ODG site. When analyses were stratified by race/ethnicity, we observed a strong, albeit imprecise, impact of distance on blood pressure among Black participants, with an increase of 100 m in distance from OGD site associated reduction of 0.21 mmHg (95% CI −3.14, 2.73) and 1.62 mmHg (95% CI −3.62, 0.38) in SBP and DBP, respectively (Table 2). Among female participants, we observed lower SBP and DBP at greater distances from well site increased and little change among male participants (Table 2).
Sensitivity analysis: ambient air pollution
As fine particulate matter pollution (PM < 2.5 µm in diameter) may adversely impact blood pressure, we considered daily PM2.5. concentration estimates on the day of the measurement for all participants. However, we found adjusting for daily PM2.5 concentrations did not change the results of the association between proximity and blood pressure measurements (Table 2).
Hypertension and proximity to oil and gas development sites
When assessing the presence of stage 1 hypertension with respect to living near (<260) or farther (260–1000 m) from the well site, we observed higher odds of hypertension (OR = 1.49, 95% 1.02, 2.18) among the residents living near the OGD site. The findings were similar when considering various restrictions and sensitivity analyses (Table 3). We observe a small, yet significant decrease in the odds of hypertension among participants for every 100 m increase in distance away from the well site.
Discussion
This study contributes to the growing literature on the health consequences for urban residents living near oil and gas extraction. Among a multiethnic cohort living atop the Las Cienegas oil field in South Los Angeles, we identified that residents living closer to the OGD site have, on average, higher blood pressure and face higher risk of stage 1 hypertension compared with residents that live farther away. This effect was more pronounced among never smokers, those within the healthy BMI category, and women residents. The association between distance to the oil well site and blood pressure was more apparent in non-smoking participants and those with lower BMI, potentially because greater BMI and smoking are known risk factors for elevated blood pressure. This study provides additional evidence of potential adverse relationship between cardiovascular health and oil drilling activities in an urban context.
Prior studies have found evidence of adverse impacts of oil and gas extraction on cardiovascular health. Communities near OGD and oil refineries are reported to have higher risks of hypertension compared with other communities farther away from these exposures [41]. A study among residents in rural Colorado found the highest SBP and DBP among people near the most OGD activity who were not taking prescription medications [32]. McKenzie and colleagues observed ~5 mmHg increase in SBP and 4 mmHg increase in DBP when the highest OGD exposed group was compared to the lowest OGD exposed group, after considering age and sex. Exposure was based on an oil and gas intensity metric within 16 km of the home and therefore not directly comparable to the metric used in this analysis. Nonetheless, we observe a similar trend among both rural residents of Colorado and urban LA, such that residents more exposed to OGD have, on average, greater blood pressure. Similarly, a study in the Niger Delta found residents chronically exposed to oil extraction and gas flaring had statistically higher SBP and DBP than the unexposed counterparts [42]. A randomized cross-sectional survey in the same region found that adults living in rural areas with OGD were nearly 5 times as likely to report hypertension compared to those living away from OGD after adjusting for socioeconomic and lifestyle factors [43].
Occupational studies suggest an association between crude oil exposures and cardiovascular health [44]. Longitudinal studies of oil cleanup workers have found duration of cleanup work associated with increased risk of myocardial infarction [45,46,47]. Additionally, the studies also found that living in proximity to the oil spill was associated with heart disease when compared to individuals living farther away [45, 46]. Among oil spill workers after the Deepwater Horizon disaster, SBP and DBP were higher with increased levels of total petroleum hydrocarbon exposure, with the strongest trend for DBP [44]. Further, higher exposure to total hydrocarbons was associated with elevated risk of newly detected hypertension, especially among workers with obesity and those who identified as Black, current smokers, and male [44]. Racism and poverty are associated with various stressors, including unemployment, financial stress, and violence, that may increase the risk of hypertension.
Oil and gas extraction sites and on-site operations typically produce a complex mixtures of air pollutants, including hydrocarbons such as benzene and diesel particulate matter [4, 11,12,13]. Hazardous compounds can be volatilized or aerosolized during extraction via active evaporating pits, flares, surface spills, processing, and transportation [12]. Research in communities atop the Las Cienegas oil field identified volatilized hydrocarbons were affecting air quality throughout the adjacent neighborhoods [19, 20] and revealed episodic peaks of air toxics likely attributable to local oil and gas operations [48]. Exposure to ambient volatile organic compounds (VOCs) has been associated with adverse cardiovascular outcomes such as emergency department visits for heart failure [49,50,51] and hypertension [52]. Additionally, oil drilling has been associated with emissions of toxic metals such as manganese and nickel [53, 54], and exposure to these metals may increase risk for hypertension [36, 55,56,57,58,59]. There may be direct impacts of environmental contaminants on biological and physiological processes, as well as psychosocial effects of living in close proximity to an OGD site. The mechanism underlying the association between OGD exposure and blood pressure, however, is still unclear. Exposure to toxic pollution and stress related to fear of potential impacts of disasters may increase the health burden in these communities, as environmental justice communities not only face additional burdens due to toxic releases, but often lack the social or financial resources to mitigate the exposures [60]. Particulate matter, noise, and stress from OGD can activate the sympathetic nervous system in humans, leading to greater oxidative stress and systemic inflammatory responses [32, 61, 62]. This may lead to autonomic nervous imbalance and endothelial dysfunction, which can then contribute to hypertension [22].
To our knowledge, this is the first study to examine the relationship between cardiovascular health in diverse urban communities and oil well sites. To date the health research OGD in the US is largely based in rural and majority non-Hispanic White communities. Our study involves a predominantly low-income community of color living in an historically underserved, environmental justice community. In this study we identify proximity to urban oil and gas development sites as a factor associated with greater blood pressure. While both SBP and DBP showed decreases with increasing distance from the well, only DBP was statistically significant. Though similar trends are observed for both SBP and DBP, it is possible that exposure to pollutants from OGD sites may target mechanisms that preferentially impact DBP, such as autonomic function, vascular reactivity, and vasoconstriction [60]. Similarly, other studies on air pollution and blood pressure in adults have reported effects limited to DBP [21, 63, 64].
Environmental justice communities can face chemical and non-chemical stressors that can pose potential cumulative and interrelated consequences for blood pressure [65]. While limited by a cross-sectional design, our study presents novel findings linking cardiovascular health effects to urban oil drilling. We cannot rule out potential confounding by unmeasured covariates or differential participation rates based on concerns about neighborhood health or environmental quality. We cannot account for lifetime residential history, individual household characteristics nor occupational exposures. Proximity is used as a proxy for exposure to pollution associated with the well sites and may represent more than just oil-related exposure (e.g., noise, stress) that cannot be disentangled from chemical exposures. Future work will include assessing neighborhood scale air pollution to better understand potential spatiotemporal patterns of regional, freeway and oil drilling related exposures. The study of environmental hazards and human exposures in nearby communities remains valuable information for public health protection, pollution prevention, and exposure reduction. The results of research can fill gaps in government data available at a local level and draw attention to local environmental health hazards.
Conclusions
Together, our findings suggest that living near urban oil drilling sites is significantly associated with greater diastolic blood pressure in South Los Angeles. This research improves understanding of impacts from living nearby drilling operations on the health and welfare of this community, which is critical to inform public health relevant strategies. As a community of predominantly low-income residents of color, these impacts raise environmental justice concerns about the effects of urban oil drilling. Reducing emissions, increasing the distance between oil operations and residents, and investments in renewable energy and energy efficiency measures that reduce reliance on fossil fuels overall—could protect the cardiovascular health of residents near oil wells.
Data availability
The survey data that support the findings of this study are not publicly available to safeguard the privacy of the participants and to maintain trust with affected communities. Data may be available from the authors upon reasonable request and with permission of the University of Southern California Institutional Review Board. Location and production of oil and gas wells is available through the California Geologic Energy Management Division.
References
US Energy Information Administration. Petroleum & other liquids: crude oil production. 2018. https://www.eia.gov/dnav/pet/pet_crd_crpdn_adc_mbblpd_a.htm.
Czolowski ED, Santoro RL, Srebotnjak T, Shonkoff SBC. Toward consistent methodology to quantify populations in proximity to oil and gas development: a national spatial analysis and review. Environ Health Perspect. 2017;125:086004.
Werner AK, Vink S, Watt K, Jagals P. Environmental health impacts of unconventional natural gas development: a review of the current strength of evidence. Sci Total Environ. 2015;505:1127–41.
Johnston JE, Lim E, Roh H. Impact of upstream oil extraction and environmental public health: a review of the evidence. Sci Total Environ. 2018;657:187–99.
Shonkoff SB, Hays J, Finkel ML. Environmental public health dimensions of shale and tight gas development. Environ Health Perspect. 2014;122:787–95.
Finkel ML, Hays J. Environmental and health impacts of ‘fracking’: why epidemiological studies are necessary. J Epidemiol Community Health. 2015;0:jech-2015–205487.
Cotton M, Charnley-Parry I. Beyond opposition and acceptance: examining public perceptions of the environmental and health impacts of unconventional oil and gas extraction. Curr Opin Environ Sci Health. 2018;3:8–13.
Chilingar GV, Endres B. Environmental hazards posed by the Los Angeles Basin urban oilfields: an historical perspective of lessons learned. Environ Geol. 2005;47:302–17.
Gamache MT, Frost PL. Urban development of oil fields in the Los Angeles Basin Area: 1983–2001. Sacramento: California Development of Conversation; 2003.
Sadd JL, Shamasunder B. Oil Extraction in Los Angeles: Health, Land Use, and Environmental Justice Consequences. In: Drilling Down: The Community Consequences of Expanded Oil Development in Los Angeles. Los Angeles, CA: Liberty Hill Foundation; 2015. pp. 7–14.
Garcia-Gonzales DA, Shonkoff SBC, Hays J, Jerrett M. Hazardous air pollutants associated with upstream oil and natural gas development: a critical synthesis of current peer-reviewed literature. Annu Rev Public Health. 2019;40:283–304.
Colborn T, Schultz K, Herrick L, Kwiatkowski C. An exploratory study of air quality near natural gas operations. Hum Ecol Risk Assess: Int J. 2014;20:86–105.
Macey GP, Breech R, Chernaik M, Cox C, Larson D, Thomas D, et al. Air concentrations of volatile compounds near oil and gas production: a community-based exploratory study. Environ Health. 2014;13:82.
Jackson RE, Gorody AW, Mayer B, Roy JW, Ryan MC, Van Stempvoort DR. Groundwater protection and unconventional gas extraction: the critical need for field‐based hydrogeological research. Groundwater. 2013;51:488–510.
Tran KV, Casey JA, Cushing LJ, Morello-Frosch R. Residential proximity to oil and gas development and birth outcomes in California: a retrospective cohort study of 2006–2015 births. Environ Health Perspect. 2020;128:067001.
Gonzalez DJX, Francis CK, Shaw GM, Cullen MR, Baiocchi M, Burke M. Upstream oil and gas production and ambient air pollution in California. Sci Total Environ. 2022;806:150298.
Johnston JE, Enebish T, Eckel SP, Navarro S, Shamasunder B. Respiratory health, pulmonary function and local engagement in urban communities near oil development. Environ Res. 2021;197:111088.
Field RA, Soltis J, Murphy S. Air quality concerns of unconventional oil and natural gas production. Environ Sci Process Impacts. 2014;16:954–69.
Johnston JE, Okorn K, Van Horne YO, Jimenez A. Changes in neighborhood air quality after idling of an urban oil production site. Environ Sci Process Impacts. 2021;23:967–80.
Okorn K, Jimenez A, Collier-Oxandale A, Johnston J, Hannigan M. Characterizing methane and total non-methane hydrocarbon levels in Los Angeles communities with oil and gas facilities using air quality monitors. Sci Total Environ. 2021;777:146194.
Brook RD, Urch B, Dvonch JT, Bard RL, Speck M, Keeler G, et al. Insights into the mechanisms and mediators of the effects of air pollution exposure on blood pressure and vascular function in healthy humans. Hypertension. 2009;54:659–67.
Brook RD. The environment and blood pressure. Cardiol Clin. 2017;35:213–21.
Giorgini P, Di Giosia P, Grassi D, Rubenfire M, Brook RD, Ferri C. Air pollution exposure and blood pressure: an updated review of the literature. Curr Pharm Des. 2016;22:28–51.
Psaty BM, Furberg CD, Kuller LH, Cushman M, Savage PJ, Levine D, et al. Association between blood pressure level and the risk of myocardial infarction, stroke, and total mortality: the cardiovascular health study. Arch Intern Med. 2001;161:1183–92.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60.
Liang R, Zhang B, Zhao X, Ruan Y, Lian H, Fan Z. Effect of exposure to PM2.5 on blood pressure: a systematic review and meta-analysis. J Hypertens. 2014;32:2130–41.
Fan F, Wang S, Zhang Y, Xu D, Jia J, Li J, et al. Acute effects of high-level PM2.5. exposure on central blood pressure. Hypertension. 2019;74:1349–56.
Dvonch JT, Kannan S, Schulz AJ, Keeler GJ, Mentz G, House J, et al. Acute effects of ambient particulate matter on blood pressure. Hypertension. 2009;53:853–9.
McGraw KE, Riggs DW, Rai S, Navas-Acien A, Xie Z, Lorkiewicz P, et al. Exposure to volatile organic compounds–acrolein, 1, 3-butadiene, and crotonaldehyde–is associated with vascular dysfunction. Environ Res. 2021;196:110903.
McGraw KE, Konkle SL, Riggs DW, Rai SN, DeJarnett NK, Xie Z, et al. Exposure to volatile organic compounds—acrolein, crotonaldehyde, and styrene—is associated with blood pressure in the Jackson Heart Study. Circulation. 2021;144:A10212.
Jemielita T, Gerton GL, Neidell M, Chillrud S, Yan B, Stute M, et al. Unconventional gas and oil drilling is associated with increased hospital utilization rates. PLoS ONE. 2015;10:e0131093.
McKenzie LM, Crooks J, Peel JL, Blair BD, Brindley S, Allshouse WB, et al. Relationships between indicators of cardiovascular disease and intensity of oil and natural gas activity in Northeastern Colorado. Environ Res. 2019;170:56–64.
California Office of Environmental Health Hazard Assessment. CalEnviroScreen 3.0: update to the California communities environmental health and screening tool. California Environmental Protection Agency, Office of Environmental Health; 2017.
Shamasunder B, Collier-Oxandale A, Blickley J, Sadd J, Chan M, Navarro S, et al. Community-based health and exposure study around urban oil developments in South Los Angeles. Int J Environ Res Public Health. 2018;15:138.
Coleman A, Freeman P, Steel S, Shennan A. Validation of the Omron 705IT (HEM-759-E) oscillometric blood pressure monitoring device according to the British Hypertension Society protocol. Blood Press Monit. 2006;11:27–32.
Xu J, Engel LS, Rhoden J, Jackson WB, Kwok RK, Sandler DP. The association between blood metals and hypertension in the GuLF study. Environ Res. 2021;202:111734.
Baguet J, Legallicier B, Auquier P, Robitail S. Updated meta-analytical approach to the efficacy of antihypertensive drugs in reducing blood pressure. Clin Drug Investig. 2007;27:735–53.
Tobin MD, Sheehan NA, Scurrah KJ, Burton PR. Adjusting for treatment effects in studies of quantitative traits: antihypertensive therapy and systolic blood pressure. Stat Med. 2005;24:2911–35.
Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT, et al. Potential U.S. population impact of the 2017 ACC/AHA high blood pressure guideline. J Am Coll Cardiol. 2018;71:109–18.
Los Angeles County Department of Public Health. 2018 Los Angeles County Health Survey. Los Angeles, CA: Office of Health Assessment and Epidemiology; 2018.
Ezejimofor MC, Uthman OA, Maduka O, Ezeabasili AC, Onwuchekwa AC, Ezejimofor BC, et al. The burden of hypertension in an oil-and gas-polluted environment: a comparative cross-sectional study. Am J Hypertens. 2016;29:925–33.
Egwurugwu JN, Nwafor A. Prolonged exposure to oil and gas flares ups the risks for hypertension. Am J Health Res. 2013;1:65–72.
Ezejimofor MC, Uthman OA, Maduka O, Ezeabasili AC, Onwuchekwa AC, Ezejimofor BC, et al. The burden of hypertension in an oil- and gas-polluted environment: a comparative cross-sectional study. Am J Hypertens. 2016;29:925–33.
Kwok RK, Jackson WB, Curry MD, Stewart PA, McGrath JA, Stenzel M, et al. Association of Deepwater Horizon oil spill response and cleanup work with risk of developing hypertension. JAMA Netw Open. 2022;5:e220108.
Strelitz J, Engel LS, Kwok RK, Miller AK, Blair A, Sandler DP. Deepwater Horizon oil spill exposures and nonfatal myocardial infarction in the GuLF STUDY. Environ Health. 2018;17:1–12.
Strelitz J, Keil AP, Richardson DB, Heiss G, Gammon MD, Kwok RK, et al. Self-reported myocardial infarction and fatal coronary heart disease among oil spill workers and community members 5 years after Deepwater Horizon. Environ Res. 2019;168:70–9.
Lee M, Park M-S, Cheong H-K. An association between oil spill clean-up work and cardiovascular disease. Ecotoxicol Environ Saf. 2020;194:110284.
Collier-Oxandale A, Wong N, Navarro S, Johnston J, Hannigan M. Using gas-phase air quality sensors to disentangle potential sources in a Los Angeles neighborhood. Atmos Environ. 2020;233:117519.
Ran J, Qiu H, Sun S, Yang A, Tian L. Are ambient volatile organic compounds environmental stressors for heart failure? Environ Pollut. 2018;242:1810–6.
Ye D, Klein M, Chang HH, Sarnat JA, Mulholland JA, Edgerton ES, et al. Estimating acute cardiorespiratory effects of ambient volatile organic compounds. Epidemiology. 2017;28:197.
Qiu H, Bai C-H, Chuang K-J, Fan Y-C, Chang T-P, Yim SH-L, et al. Association of cardiorespiratory hospital admissions with ambient volatile organic compounds: evidence from a time-series study in Taipei, Taiwan. Chemosphere. 2021;276:130172.
Xu J, Niehoff NM, White AJ, Werder EJ, Sandler DP. Fossil-fuel and combustion-related air pollution and hypertension in the Sister Study. Environ Pollut. 2022;315:120401.
Quist AJL, Van Horne YO, Farzan SF, Johnston JE. Metal exposures in residents living near an urban oil drilling site in Los Angeles, California. Environ Sci Technol. 2022;56:15981–9.
Barker C. Origin, composition and properties of petroleum. In: Donaldson EC, Chilingarian GV, Yen TF, editors. Developments in Petroleum Science. Vol. 17. New York: Elsevier; 1985. pp 11–45.
Lee B-K, Kim Y. Relationship between blood manganese and blood pressure in the Korean general population according to KNHANES 2008. Environ Res. 2011;111:797–803.
Chen H, Cui Z, Lu W, Wang P, Wang J, Zhou Z, et al. Geographical, sex, age, and seasonal differences in serum manganese status among Chinese adults with hypertension. Biol Trace Elem Res. 2022;201:41–50.
Xu J, White AJ, Niehoff NM, O’Brien KM, Sandler DP. Airborne metals exposure and risk of hypertension in the Sister Study. Environ Res. 2020;191:110144.
Afridi HI, Kazi TG, Talpur FN, Arain S, Arain SS, Kazi N, et al. Distribution of arsenic, cadmium, lead, and nickel levels in biological samples of Pakistani hypertensive patients and control subjects. Clin Lab. 2014;60:1309–18.
Ma J, Zhang H, Zheng T, Zhang W, Yang C, Yu L, et al. Exposure to metal mixtures and hypertensive disorders of pregnancy: a nested case-control study in China. Environ Pollut. 2022;306:119439.
Johnston J, Cushing L. Chemical exposures, health, and environmental justice in communities living on the fenceline of industry. Curr Environ Health Rep. 2020;7:48–57.
Donaldson K, Stone V, Seaton A, MacNee W. Ambient particle inhalation and the cardiovascular system: potential mechanisms. Environ Health Perspect. 2001;109:523–7.
Wirtz PH, von Känel R. Psychological stress, inflammation, and coronary heart disease. Curr Cardiol Rep. 2017;19:1–10.
Liu L, Ruddy T, Dalipaj M, Poon R, Szyszkowicz M, You H, et al. Effects of indoor, outdoor, and personal exposure to particulate air pollution on cardiovascular physiology and systemic mediators in seniors. J Occup Environ Med. 2009;51:1088–98.
Williams R, Brook R, Bard R, Conner T, Shin H, Burnett R. Impact of personal and ambient-level exposures to nitrogen dioxide and particulate matter on cardiovascular function. Int J Environ Health Res. 2012;22:71–91.
Peters JL, Fabian MP, Levy JI. Epidemiologically-informed cumulative risk hypertension models simulating the impact of changes in metal, organochlorine, and non-chemical exposures in an environmental justice community. Environ Res. 2019;176:108544.
Acknowledgements
This work was supported in part by a grant from the National Institute of Environmental Health Sciences (ES033478 and ES027695). Thank you to all our partners at Esperanza Community Housing and Redeemer Community Partnership, along with Ruth Andrade, Alejandra Castillo, Deisy Gutierrez, Amanda Jimenez, Kelly Koh, Esther Lim, Leticia Ortiz, Veronica Ponce de Leon, Toby Rodriguez, Sandra Serrano, Blanca Valdez and Nicole Wong.
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium.
Author information
Authors and Affiliations
Contributions
JEJ and BS are the principal investigators of this study and together with SN conceptualized the Health and Air Pollution study, developed protocols, obtained funding and ethics approval and supervised all study operations. SN and JEJ oversaw participants data collection and data entry, implemented protocols, and coordinated with community sites. AJLQ led the data analysis and support manuscript writing. SFF advised on the blood pressure protocols and data analysis. JEJ and AJLQ wrote the first draft of the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Johnston, J.E., Quist, A.J.L., Navarro, S. et al. Cardiovascular health and proximity to urban oil drilling in Los Angeles, California. J Expo Sci Environ Epidemiol (2023). https://doi.org/10.1038/s41370-023-00589-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41370-023-00589-z